NEWS - JULY 2019
CONSULTATION RE. AGEING
Scope of Inquiry
While life span has increased over recent decades, health span, the period of time people live in good health, has generally not kept pace, and so older people are living longer with ill health. This inquiry will investigate how approaches from science and technology could be used to increase health span, to mitigate some of the negative effects of ageing, and to support older people living with poor health.
25 July 2019
The House of Lords Science and Technology Committee launches an inquiry into Ageing: Science, Technology and Healthy Living.
Background
Life span has increased over recent decades, but health span, the period of time people live in good health, has generally not kept pace, and so older people are living longer with ill health. This increased duration of ill health, both physical and psychological, and often compounded by loneliness, can be challenging for individuals; and the increasing number of people affected is placing pressure on health services and social care, threatening to overwhelm the funding mechanisms, and failing those in need.
Increasing health span has been adopted as a policy objective by the UK Government in the Industrial Strategy’s "Ageing Society" Grand Challenge, which aims to ensure that people can enjoy at least five extra healthy, independent years of life by 2035. This House of Lords inquiry will seek to determine whether the Government's ambition to increase health span is achievable in principle, and which approaches may be most successful in practice.
The Committee invites submissions, with practical examples where possible, on the topics mentioned below.
Scope
Chairman's Comments
Chair of the Committee, Lord Patel, said:
"The Government wants to increase the health span of the population, which would mean that people could live independently for longer, with better health and well-being and would reduce pressure on services and finances.
"The Committee will explore how achievable the Government’s aim is by looking at what treatments and technologies could be available to address ageing and ageing-related diseases, and at the scientific basis for public health advice about healthy lifestyle. The Committee will also explore the policies that would be needed to achieve the aim of increased health span, and the policies that would be needed to support a healthier, older population."
Timeline
The Committee is inviting written evidence on the issue, to be received by Friday 20 September 2019, and will start taking oral evidence on the inquiry in October.
https://www.parliament.uk/business/committees/committees-a-z/lords-select/science-and-technology-committee/inquiries/parliament-2017/ageing-science-technology-and-healthy-living/
Scope of Inquiry
While life span has increased over recent decades, health span, the period of time people live in good health, has generally not kept pace, and so older people are living longer with ill health. This inquiry will investigate how approaches from science and technology could be used to increase health span, to mitigate some of the negative effects of ageing, and to support older people living with poor health.
25 July 2019
The House of Lords Science and Technology Committee launches an inquiry into Ageing: Science, Technology and Healthy Living.
- Call for evidence: Ageing: Science, Technology and Healthy Living ( PDF 112 KB)
- Send a written submission
- Inquiry: Ageing: Science, Technology and Healthy Living
- Science and Technology Select Committee (Lords)
Background
Life span has increased over recent decades, but health span, the period of time people live in good health, has generally not kept pace, and so older people are living longer with ill health. This increased duration of ill health, both physical and psychological, and often compounded by loneliness, can be challenging for individuals; and the increasing number of people affected is placing pressure on health services and social care, threatening to overwhelm the funding mechanisms, and failing those in need.
Increasing health span has been adopted as a policy objective by the UK Government in the Industrial Strategy’s "Ageing Society" Grand Challenge, which aims to ensure that people can enjoy at least five extra healthy, independent years of life by 2035. This House of Lords inquiry will seek to determine whether the Government's ambition to increase health span is achievable in principle, and which approaches may be most successful in practice.
The Committee invites submissions, with practical examples where possible, on the topics mentioned below.
Scope
- The scientific understanding of the ageing process, and how these areas of research could lead to treatments for delaying or managing the negative effects of ageing.
- Technologies that can improve health and wellbeing in old age, and technologies that can enable independent living in old age.
- Opportunities for the UK to commercialise discoveries and innovations relating to healthier ageing
- The policy implications of a healthier older population.
Chairman's Comments
Chair of the Committee, Lord Patel, said:
"The Government wants to increase the health span of the population, which would mean that people could live independently for longer, with better health and well-being and would reduce pressure on services and finances.
"The Committee will explore how achievable the Government’s aim is by looking at what treatments and technologies could be available to address ageing and ageing-related diseases, and at the scientific basis for public health advice about healthy lifestyle. The Committee will also explore the policies that would be needed to achieve the aim of increased health span, and the policies that would be needed to support a healthier, older population."
Timeline
The Committee is inviting written evidence on the issue, to be received by Friday 20 September 2019, and will start taking oral evidence on the inquiry in October.
https://www.parliament.uk/business/committees/committees-a-z/lords-select/science-and-technology-committee/inquiries/parliament-2017/ageing-science-technology-and-healthy-living/
COMMUNITY PHARMACIES - COMING IN OCTOBER
Community Pharmacies are in a similar position to General Practice. Core income is shrinking and Pharmacies need to consider new ways to make money.
Under a new contracting deal, a national scheme to offer consultations is due to start from October.
Patients could be referred to Pharmacies by GPs, the NHS 111 service and possibly also by Urgent Care Centres and Emergency Departments.
Medicines use reviews [MUR] currently carried out by Community Pharmacies will be done instead by ‘practice based Pharmacists’ under the new name of “structured medication reviews”, but Pharmacies will be able to offer a broader range of clinical services, such as routine monitoring of patients on repeat medication, which could potentially reduce General Practice workload.
Community Pharmacies are in a similar position to General Practice. Core income is shrinking and Pharmacies need to consider new ways to make money.
Under a new contracting deal, a national scheme to offer consultations is due to start from October.
Patients could be referred to Pharmacies by GPs, the NHS 111 service and possibly also by Urgent Care Centres and Emergency Departments.
Medicines use reviews [MUR] currently carried out by Community Pharmacies will be done instead by ‘practice based Pharmacists’ under the new name of “structured medication reviews”, but Pharmacies will be able to offer a broader range of clinical services, such as routine monitoring of patients on repeat medication, which could potentially reduce General Practice workload.
SOCIAL PRESCRIBING LINK WORKERS: Reference guide for Primary Care Networks
7 pages
NHS England has published a guide for Primary Care Networks (PCNs) introducing the new role of social prescribing link worker into their teams.
7 pages
NHS England has published a guide for Primary Care Networks (PCNs) introducing the new role of social prescribing link worker into their teams.
|
LTP SPENDING ALLOCATIONS
NHS England - Board Paper - 24 pages Community and young people’s mental health services will receive the lion’s share of the sector’s long-term plan funding, while inpatient services are promised very little. |
CCGs SCORES FOR PATIENT ENGAGEMENT
---- go to the link below, put in your post code, and the ppe scores are in the last column, on the right.
- CCGs get their scores for patient engagement.
- CCGs are obliged to report on their performance against a patient and community engagement indicator as part of the improvement and assessment framework (IAF).
---- go to the link below, put in your post code, and the ppe scores are in the last column, on the right.
A much-anticipated review of community nursing by HEE has been ditched after internal complaints were raised by members of the advisory panel.
Health Education England has decided not to publish a review it has carried out of community nursing over the past year, saying the work will instead feed into wider workforce plans.
When launching the review in 2018, HEE had said it was “essential” to understand why training places were not being filled and support a more flexible workforce.
According to multiple senior sources, the decision has come after two members of its steering group pulled out of the review due to serious criticisms over the quality and focus of the report. Also, there were requests from other members of the group that the report not be published.
Organisations included in the steering group were NHS Improvement, NHS England, the Nursing and Midwifery Council, the Royal College of Nursing, the Council of Deans, the Queen’s Nursing Institute, and provider trust representatives.
It comes after concerns from members of the steering group were revealed in March, including that the work was heavily “based on anecdote” and “conversations”.
Health Education England has decided not to publish a review it has carried out of community nursing over the past year, saying the work will instead feed into wider workforce plans.
When launching the review in 2018, HEE had said it was “essential” to understand why training places were not being filled and support a more flexible workforce.
According to multiple senior sources, the decision has come after two members of its steering group pulled out of the review due to serious criticisms over the quality and focus of the report. Also, there were requests from other members of the group that the report not be published.
Organisations included in the steering group were NHS Improvement, NHS England, the Nursing and Midwifery Council, the Royal College of Nursing, the Council of Deans, the Queen’s Nursing Institute, and provider trust representatives.
It comes after concerns from members of the steering group were revealed in March, including that the work was heavily “based on anecdote” and “conversations”.
|
DUTY TO CONSULT
21 pages This publication is designed to provide a comprehensive understanding of the statutory duties of NHS providers and Commissioners, in relation to the provision of health care. |
It deals with the duties to involve, engage and consult the public in the development of services, and clarifies the rights of the public to be involved at every level when significant changes are planned for services. In particular, the document makes it clear that it is unlawful for NHS bodies to disregard the public’s views when NHS services and systems are being redesigned.
Patients must always be in the centre of NHS planning, organisation and services’ provision, wherever and whenever changes are planned for our services.
Patients must always be in the centre of NHS planning, organisation and services’ provision, wherever and whenever changes are planned for our services.
|
SOCIAL CARE: PAYING FOR CARE HOME PLACES AND DOMICILIARY CARE (ENGLAND)
38 pages This House of Commons Library briefing paper sets out how individuals are assessed for local authority funding support towards the costs of their social care for 2019/20 |
Summary:
Below are some of the key metrics for the social care means-test for 2019/20:
In order to determine eligibility for local authority funding support towards social care costs, someone’s capital is assessed against the upper limit. For care home residents only, their capital can include the value of their home but this has to be disregarded from the means-test if certain conditions are met or if a local authority decides to exercise its discretion to disregard it.
Those recipients of social care with capital below the upper limit are eligible for local authority funding support toward the cost, but they are still required to contribute any income they receive (except disregarded income, such as earnings). There is no limit of the amount of income someone has to contribute over their lifetime. They are allowed to retain a certain amount each week for personal expenses and (if applicable) household bills.
A deferred payments agreement may be offered by a local authority, which can avoid the need for a care home resident to sell their home during their lifetime. In addition, third (or in some limited cases, first) party top-ups can be used to finance a more expensive care home setting than a local authority would normally fund.
Below are some of the key metrics for the social care means-test for 2019/20:
- Upper capital limit - £23,250
- Lower capital limit - £14,250
- Personal Expenses Allowance - £24.90 per week
- Minimum Income Guarantee - depends on circumstances, see Annex of the pdf document
In order to determine eligibility for local authority funding support towards social care costs, someone’s capital is assessed against the upper limit. For care home residents only, their capital can include the value of their home but this has to be disregarded from the means-test if certain conditions are met or if a local authority decides to exercise its discretion to disregard it.
Those recipients of social care with capital below the upper limit are eligible for local authority funding support toward the cost, but they are still required to contribute any income they receive (except disregarded income, such as earnings). There is no limit of the amount of income someone has to contribute over their lifetime. They are allowed to retain a certain amount each week for personal expenses and (if applicable) household bills.
A deferred payments agreement may be offered by a local authority, which can avoid the need for a care home resident to sell their home during their lifetime. In addition, third (or in some limited cases, first) party top-ups can be used to finance a more expensive care home setting than a local authority would normally fund.
LEGISLATION EMPOWERING THE NHS, ETC.
In the face of ever more bewildering change, I am receiving more requests for sources of info. on what empowered which bit of the NHS to do what.
Best overall outline seems to be in the Explanatory Notes to the 2012 Act.
The link to this is here: http://www.legislation.gov.uk/ukpga/2012/7/notes
In the face of ever more bewildering change, I am receiving more requests for sources of info. on what empowered which bit of the NHS to do what.
Best overall outline seems to be in the Explanatory Notes to the 2012 Act.
The link to this is here: http://www.legislation.gov.uk/ukpga/2012/7/notes
NHSE and NHSI AMALGAMATION AND STAFF REDUCTION
NHSE and NHSI set to scrap one in seven posts. NHS England and Improvement are beginning the third and largest phase of the restructure bringing the two organisations together, which is expected in total to remove about 15 per cent of posts.
They today launched a consultation on “phase three” of their joint working restructure programme. This phase covers all staff on Agenda for Change contracts or equivalents. The more senior staff, have been covered in previous phases.
In total, the restructure – including all three phases – is expected to reduce the current number of posts by around 1,200, estimated to be a reduction of around 15.2 per cent.
According to the consultation document, the estimated number of people put at risk of redundancy today in phase three is 966.
The current figures are not final, in part because structures for the “people” directorate and posts linked to NHSX – the digital division jointly reporting to the Department of Health and Social Care – are not complete.
NHSE and NHSI set to scrap one in seven posts. NHS England and Improvement are beginning the third and largest phase of the restructure bringing the two organisations together, which is expected in total to remove about 15 per cent of posts.
They today launched a consultation on “phase three” of their joint working restructure programme. This phase covers all staff on Agenda for Change contracts or equivalents. The more senior staff, have been covered in previous phases.
In total, the restructure – including all three phases – is expected to reduce the current number of posts by around 1,200, estimated to be a reduction of around 15.2 per cent.
According to the consultation document, the estimated number of people put at risk of redundancy today in phase three is 966.
The current figures are not final, in part because structures for the “people” directorate and posts linked to NHSX – the digital division jointly reporting to the Department of Health and Social Care – are not complete.
|
HEALTH AND WELLBEING BOARDS
40 pages This resource captures the achievements, challenges and learning from 22 effective Health and Wellbeing Boards (HWBs) across the country, all of which are making good This report refers to the sample of 22 HWBs identified, rather than all 153 HWBs throughout the country. Many other HWBs, however, will also have the same characteristics as the ones featured in this publication. |
|
A GUIDE TO HEALTHWATCH POWERS TO ENTER AND VIEW HEALTH AND CARE SERVICES
8 pages Healthwatch has a legal power to visit health and social care services and see them in action. This power to Enter and View services offers a way for Healthwatch to meet some of their statutory functions and allows them to identify what is working well with services and where they could be improved. |
NHS 'PATHWAYS' - Issues
Patients die after multiple warnings about the national 999 IT system were dismissed ...
5 pages
Patients die after multiple warnings about the national 999 IT system were dismissed ...
5 pages
|
HOW IS YOUR CCG RATED?
Sixty-three Clinical Commissioning Groups have seen their overall performance ratings change over the past year, according to NHS England’s latest assessment framework. The national governing body has published its Annual Ratings for 2018-19, which represent how well CCGs have performed across 50 different areas. These include financial stability, leadership and care quality services. They are then judged to fall within one of four categories – Outstanding, Good, Requires Improvement or Inadequate. |
|
THE IMPACT OF RECENT BENEFIT CHANGES ON VULNERABLE PEOPLE
The Impact of recent benefit changes on vulnerable people House of Lords - 27 June 2019 |
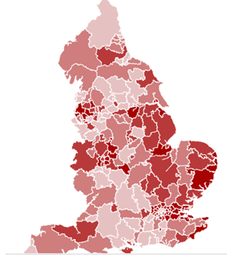
GPs OF AGE TO RETIRE
More than a third of the full-time equivalent (FTE) GP workforce is aged 55 or over, in nearly one in 10 CCGs.
More than a third of the full-time equivalent (FTE) GP workforce is aged 55 or over, in nearly one in 10 CCGs.
|
Evidence from GPonline suggests that the vast majority of GPs aged over 55, plan to quit the profession within five years - leaving some CCGs at imminent risk of severe workforce shortages. Mapped data from NHS Digital reveals the parts of England most at risk from the impact of an ageing GP workforce. |
CCG MERGERS - REQUIREMENT TO DEMONSTRATE CONSULTATION WITH LOCAL HEALTHWATCHES
Ellie Reeves - Labour, Lewisham West and Penge
To ask the Secretary of State for Health and Social Care, what plans he has to (a) monitor and (b) evaluate the merit of mergers between clinical commissioning groups.
Ellie Reeves - Labour, Lewisham West and Penge
To ask the Secretary of State for Health and Social Care, what plans he has to (a) monitor and (b) evaluate the merit of mergers between clinical commissioning groups.
- Hansard source (Citation: HC Deb, 5 July 2019, cW)
PRIVATE PROVIDER OF NHS SERVICES
01 July 2019
NHS spend with the company fell from £293.3m to £272.2m, while NHS revenues were down 7.2 per cent and NHS-funded admissions fell 8.7 per cent to 92,674.
The company’s revenue of £931m was comprised 29.2 per cent of NHS payers, while 18.7 per cent was from self-paying patients and 46.5 per cent came from private medical insurance.
The accounts, published this week, said the decline in NHS business made 2018 “a difficult year” across the sector. It said there were fewer NHS admissions “as NHS commissioners deal with on-going financial pressures through triage and changes to referral processes”.
Orthopaedic care was particularly badly hit, the company reported.
Another part of the report said NHS trusts had become less willing to outsource work “due to the relaxation of penalties linked to referral to treatment times”.
Spire operates from 39 different hospitals across the UK.
01 July 2019
- profits fall at Spire Healthcare as CEO cites “volatility” in NHS market
- NHS spend with the company falls 8.7 per cent year-on-year, annual accounts published this week reveal
- Orthopaedics in particular declines while trusts outsourcing less
NHS spend with the company fell from £293.3m to £272.2m, while NHS revenues were down 7.2 per cent and NHS-funded admissions fell 8.7 per cent to 92,674.
The company’s revenue of £931m was comprised 29.2 per cent of NHS payers, while 18.7 per cent was from self-paying patients and 46.5 per cent came from private medical insurance.
The accounts, published this week, said the decline in NHS business made 2018 “a difficult year” across the sector. It said there were fewer NHS admissions “as NHS commissioners deal with on-going financial pressures through triage and changes to referral processes”.
Orthopaedic care was particularly badly hit, the company reported.
Another part of the report said NHS trusts had become less willing to outsource work “due to the relaxation of penalties linked to referral to treatment times”.
Spire operates from 39 different hospitals across the UK.
INVESTIGATION INTO NHS PROPERTY SERVICES LIMITED
June 2019 - 2 pages
https://www.nao.org.uk/press-release/investigation-into-nhs-property-services-limited/
Today’s report by the National Audit Office has found that NHS Property Services Limited (the Service) lacks the powers it needs to make its tenants sign lease agreements and pay their rent, which has contributed to increasing levels of outstanding debt.
The Service was established in December 2011 to manage, maintain and improve NHS properties in England and facilities previously owned by Strategic Health Authorities and Primary Care Trusts. It operates 2,900 properties with an estimated value of £3.8 billion, and has approximately 6,950 tenants.
The Service has no effective way of getting tenants to sign formal rental agreements. Since 2013-14 the percentage of tenants without leases has increased from nearly two-thirds to 70%. The Service has improved the quality of data it holds and introduced a new billing system in 2017, but many bills are still disputed, particularly by tenants without rental agreements.
The Service does not have the same powers as a commercial landlord for NHS tenants, limiting its ability to take action when bills are not paid. Action against non-NHS tenants, including GPs, must be approved by the Department on a case-by-case basis.
Outstanding debt has almost tripled, to £576 million, and tenants are taking much longer to pay their debts. In 2018-19, the Service only recovered 58.4p for every £1 it billed. Although GPs only occupy 18% of properties, they owe 30% of the current outstanding debt. Between 2014-15 and 2018-19, the Service wrote off £110 million of debt and a new arbitration process for resolving disputed bills is not working effectively.
The Service has met most of its estates management objectives. By March 2019, it had sold 410 excess properties at a value of £347 million, and invested £447 million in upgrading, maintaining and developing new facilities. The Service has also reduced the 2,400 separate facilities management service arrangements it inherited to around 50 contracts. However, in 2017 the Department estimated the Service had a backlog of maintenance work worth £1 billion.
The Service has not met the Department’s goal for it to become financially self-reliant. Between 2013-14 and 2018-19, it reduced its direct operating costs by £51 million. However, it recorded a loss in each financial year, with total losses of £1,010 million, including losses of £565 million that resulted from the revaluation of assets. The Service’s seven directors received total bonuses of £206,000 in 2018-19.
The NAO recommends that the Department, in collaboration with the Service and NHS bodies should: ensure that the Service and all of its tenants agree tenancy details and amounts by the end of March 2020; and put in place a process to ensure that all billing disputes are settled within 90 days. The Service should develop quality metrics for the accuracy of billing.
June 2019 - 2 pages
https://www.nao.org.uk/press-release/investigation-into-nhs-property-services-limited/
Today’s report by the National Audit Office has found that NHS Property Services Limited (the Service) lacks the powers it needs to make its tenants sign lease agreements and pay their rent, which has contributed to increasing levels of outstanding debt.
The Service was established in December 2011 to manage, maintain and improve NHS properties in England and facilities previously owned by Strategic Health Authorities and Primary Care Trusts. It operates 2,900 properties with an estimated value of £3.8 billion, and has approximately 6,950 tenants.
The Service has no effective way of getting tenants to sign formal rental agreements. Since 2013-14 the percentage of tenants without leases has increased from nearly two-thirds to 70%. The Service has improved the quality of data it holds and introduced a new billing system in 2017, but many bills are still disputed, particularly by tenants without rental agreements.
The Service does not have the same powers as a commercial landlord for NHS tenants, limiting its ability to take action when bills are not paid. Action against non-NHS tenants, including GPs, must be approved by the Department on a case-by-case basis.
Outstanding debt has almost tripled, to £576 million, and tenants are taking much longer to pay their debts. In 2018-19, the Service only recovered 58.4p for every £1 it billed. Although GPs only occupy 18% of properties, they owe 30% of the current outstanding debt. Between 2014-15 and 2018-19, the Service wrote off £110 million of debt and a new arbitration process for resolving disputed bills is not working effectively.
The Service has met most of its estates management objectives. By March 2019, it had sold 410 excess properties at a value of £347 million, and invested £447 million in upgrading, maintaining and developing new facilities. The Service has also reduced the 2,400 separate facilities management service arrangements it inherited to around 50 contracts. However, in 2017 the Department estimated the Service had a backlog of maintenance work worth £1 billion.
The Service has not met the Department’s goal for it to become financially self-reliant. Between 2013-14 and 2018-19, it reduced its direct operating costs by £51 million. However, it recorded a loss in each financial year, with total losses of £1,010 million, including losses of £565 million that resulted from the revaluation of assets. The Service’s seven directors received total bonuses of £206,000 in 2018-19.
The NAO recommends that the Department, in collaboration with the Service and NHS bodies should: ensure that the Service and all of its tenants agree tenancy details and amounts by the end of March 2020; and put in place a process to ensure that all billing disputes are settled within 90 days. The Service should develop quality metrics for the accuracy of billing.
|
PRIMARY CARE - DIGITALISATION
40 pages The attached describes the proposals to:
|
BREXIT
Letter to the Secretary of State, Rt. Hon. Steve Barclay, MP from Chief Negotiator, The European Commission
Brussels, 18 June 2019 ... 2 pages
Letter to the Secretary of State, Rt. Hon. Steve Barclay, MP from Chief Negotiator, The European Commission
Brussels, 18 June 2019 ... 2 pages
PRIMARY CARE NETWORKS
- An update on progress with implementation of the five-year deal agreed, earlier this year, says the number of GP Practices choosing not to join PCNs has been falling steadily - but NHS England confirmed it did not expect any change of heart among the remaining 26 Practices.
- The document confirms that nearly one in 10 PCNs are smaller than the standard 30,000- to 50,000-patient range envisaged in the five-year contract agreement.
- Of 1,259 PCNs set up across England, 111 have fewer than 30,000 patients, NHS England has confirmed - with 26 of these below the 27,000 mark and two with less than 20,000 patients.