NEWS - JANUARY / FEBRUARY / MARCH 2018
|
GOVERNMENT, HEALTH AND SOCIAL CARE
February 2018 ... 44 pages ---- Government command paper, responding to the Lords’ Select Committee Report on long-term sustainability of the NHS and adult social care. |
NEW GUIDANCE ON MEDICINES MANAGEMENT FOR NURSING ASSOCIATES PUBLISHED
20 February 2018
Advisory guidance setting out expectations for nursing associates who administer medicines to patients has been launched by Health Education England (HEE) today.
The guidance is aimed at employers, trainers, supervisors, training providers, nursing associates and patients and sets out best practice for employers delivering medicines management training.
20 February 2018
Advisory guidance setting out expectations for nursing associates who administer medicines to patients has been launched by Health Education England (HEE) today.
The guidance is aimed at employers, trainers, supervisors, training providers, nursing associates and patients and sets out best practice for employers delivering medicines management training.
CARE GAPS FOR THOUSANDS OF PATIENTS WHO CHOOSE GP AWAY FROM HOME
20 February 2018 ... 2 pages
There may be gaps in primary care for more than 14,000 people who are registered with GP practices outside their area, HSJ has found.
20 February 2018 ... 2 pages
There may be gaps in primary care for more than 14,000 people who are registered with GP practices outside their area, HSJ has found.
PHARMACIES - STAY WELL CAMPAIGN
NHS England’s Stay Well Pharmacy campaign, which encourages the public to ask community pharmacy teams for advice on minor health concerns, has launched this week.
Community pharmacies should receive a briefing pack and resources including posters from NHS England this week.
The campaign uses posters, leaflets, social media activity and television advertising to raise awareness. Running until 31 March 2018, the campaign encourages people to use pharmacies rather than visiting their GP as a first port of call.
Details can be found here: http://psnc.org.uk/our-news/stay-well-pharmacy-campaign-launches/
NHS England’s Stay Well Pharmacy campaign, which encourages the public to ask community pharmacy teams for advice on minor health concerns, has launched this week.
Community pharmacies should receive a briefing pack and resources including posters from NHS England this week.
The campaign uses posters, leaflets, social media activity and television advertising to raise awareness. Running until 31 March 2018, the campaign encourages people to use pharmacies rather than visiting their GP as a first port of call.
Details can be found here: http://psnc.org.uk/our-news/stay-well-pharmacy-campaign-launches/
|
GUIDANCE ON JOINT WORKING FOR SHORT NOTICE CLOSURES
4 pages NHS England has published guidance for any organisation involved in a short notice closure, so it can take appropriate and timely action in supporting patients and make sure they get the care and treatment they deserve. Foreword - Commissioning Body - Local Authorities . Provider/Service - Care Quality Commission . NHS Improvement . NHS England |
|
VOLUNTEERING IN GENERAL PRACTICE - Opportunities and Insights
By: Helen Gilburt, David Buck and Jane South ... February 2018 - 73 pages Introduction . Approaches to Volunteering in General Practice . Examples from Practice . Make It Happen . Choosing and Developing an Approach . Supporting and Managing Volunteers Strategic Issues . The Value of Volunteering in General Practice . Conclusions |
|
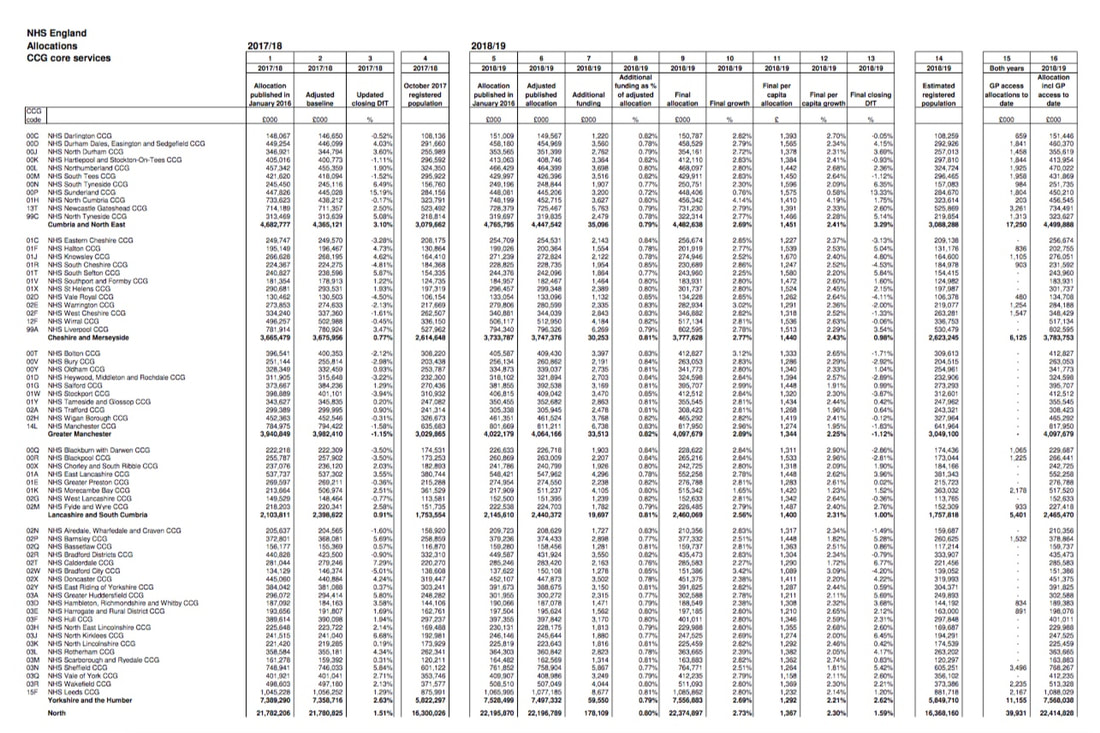
WHO GETS WHAT ...
Details of additional CCG funding allocations and revised target allocations for 2018/2019. https://www.networks.nhs.uk/networks/news/revised-ccg-allocations-2018-19 |
|
ACS now ICS ... Rebranded - accountable care systems - revised planning guidance
6 February 2018 NHS England has rebranded the existing ACS areas “integrated care systems” (ICS) in planning guidance for 2018/19 published last week. The eight existing shadow ACSs and the devolved health systems in Manchester and Surrey will be known as ICSs in future. The document stresses the need for greater engagement with patients and the public. |
MISDIRECTED MATERIAL - CONFUSION
More than 18 months after the DH and NHS England were informed that a huge backlog of clinical correspondence had been found, a report from the House of Commons' Public Accounts Committee says MPs are 'deeply unimpressed by the lack of grip NHS England still has' on the problem.
The report warns that almost 2,000 patients are still being assessed by NHS England to determine whether they have been harmed by the mishandling of correspondence, and MPs said NHS England had 'assumed without evidence' that a further 102,000 patients had not suffered harm.
MPs were 'dismayed' to be told last month, that a further backlog of more than 160,000 records had been identified - on top of 709,000 identified initially.
------------------------------------------------
GP leaders have blamed confusion around the outsourcing of NHS primary care support services to Capita for thousands of items of clinical correspondence being misdirected.
NHS England continues to receive between 5,000 and 10,000 items of clinical correspondence a month that have been sent in error by GP practices to Capita, according to a report by the National Audit Office (NAO).
https://www.nao.org.uk/wp-content/uploads/2018/02/Investigation-into-clinical-correspondence-handling-in-the-NHS.pdf
The work of the National Incident Team report -
3.8 Figure 5 shows that by 13 November 2017 the NIT had identified a total of 373,868 pieces of clinical correspondence.
These included, for example, pathology reports, coroners’ reports, discharge notifications, patient invitation letters, treatment/diagnosis notes, test results and documents/referrals marked ‘urgent’. It also identified some non-clinical documents such as staff documentation and patient questionnaires.
The clinical correspondence that transferred from closed PCS centres was found to include material from centres run by NHS England (91,953 items), NHS SBS (12,053 items) and Serco (3,196 items). The 21 boxes from NHS SBS showed no evidence of having been processed. Of the remaining 139 boxes, 43 boxes showed no evidence of processing or had been processed.
More than 18 months after the DH and NHS England were informed that a huge backlog of clinical correspondence had been found, a report from the House of Commons' Public Accounts Committee says MPs are 'deeply unimpressed by the lack of grip NHS England still has' on the problem.
The report warns that almost 2,000 patients are still being assessed by NHS England to determine whether they have been harmed by the mishandling of correspondence, and MPs said NHS England had 'assumed without evidence' that a further 102,000 patients had not suffered harm.
MPs were 'dismayed' to be told last month, that a further backlog of more than 160,000 records had been identified - on top of 709,000 identified initially.
------------------------------------------------
GP leaders have blamed confusion around the outsourcing of NHS primary care support services to Capita for thousands of items of clinical correspondence being misdirected.
NHS England continues to receive between 5,000 and 10,000 items of clinical correspondence a month that have been sent in error by GP practices to Capita, according to a report by the National Audit Office (NAO).
https://www.nao.org.uk/wp-content/uploads/2018/02/Investigation-into-clinical-correspondence-handling-in-the-NHS.pdf
The work of the National Incident Team report -
3.8 Figure 5 shows that by 13 November 2017 the NIT had identified a total of 373,868 pieces of clinical correspondence.
These included, for example, pathology reports, coroners’ reports, discharge notifications, patient invitation letters, treatment/diagnosis notes, test results and documents/referrals marked ‘urgent’. It also identified some non-clinical documents such as staff documentation and patient questionnaires.
The clinical correspondence that transferred from closed PCS centres was found to include material from centres run by NHS England (91,953 items), NHS SBS (12,053 items) and Serco (3,196 items). The 21 boxes from NHS SBS showed no evidence of having been processed. Of the remaining 139 boxes, 43 boxes showed no evidence of processing or had been processed.
DEADLINE BROUGHT FORWARD FOR EXTENDED GP ACCESS TO COVER ENGLAND
In an update to its plans for 2018/19, NHS England and NHS Improvement said it wanted everyone in England to have access to extended GP services by 01 October 2018, instead of the end of March 2019, as originally planned.
Extended GP services involves providing access to pre-bookable and same-day GP appointments in the evening (after 6.30pm) and at weekends, although these are not necessarily at patients' own practice.
The document revealed that 52% of the country now has access to these services - the original target was for 40% of the country to be covered by April 2018.
In an update to its plans for 2018/19, NHS England and NHS Improvement said it wanted everyone in England to have access to extended GP services by 01 October 2018, instead of the end of March 2019, as originally planned.
Extended GP services involves providing access to pre-bookable and same-day GP appointments in the evening (after 6.30pm) and at weekends, although these are not necessarily at patients' own practice.
The document revealed that 52% of the country now has access to these services - the original target was for 40% of the country to be covered by April 2018.
OVERSEAS RECRUITMENT OF GPs ... GP Forward View’
The move to expand overseas recruitment follows successful pilots in Lincolnshire, Essex and Cumbria, which have involved EEA Doctors.
Lincolnshire is the most advanced of the current pilot schemes. Dr Kieran Sharrock, Lincolnshire LMC Medical Director, explains that it was established in Spring 2016 and attracted 260 expressions of interest. Now, 26 Doctors are working in 16 Practices in the region.
The fully-qualified GPs have come from seven EU countries: France, Spain, Italy, Poland, Romania, Lithuania and Croatia, having gone trough eligibility language assessment and face-to-face interviews with Practices.
To meet all the regulatory requirements for entry on to the national performers list, the Doctors in the Lincolnshire scheme first attended a 12-week residential intensive training programme at a campus in Poland. ‘This aimed to get candidates’ English language and knowledge and skills around basic NHS processes up to scratch,’ says Dr Sharrock. ‘They were given Bursaries to attend.’
Each Doctor completes a learning needs assessment, which feeds into their individualised personal development plan. They also have an individual clinical educational plan, which follows a similar blueprint to the MRCGP, covering areas including: clinical updates, screening and immunisation updates, medicines management and prescribing, regulatory aspects, primary care administration, unscheduled care and the role of allied health professionals.
In addition, the recruits have undertaken mandatory online training requirements, such as infection control, information governance and safeguarding
The GPs will be mentored by their recruiting practices, for which surgeries have been given a small amount of funding, Dr Sharrock adds.
The move to expand overseas recruitment follows successful pilots in Lincolnshire, Essex and Cumbria, which have involved EEA Doctors.
Lincolnshire is the most advanced of the current pilot schemes. Dr Kieran Sharrock, Lincolnshire LMC Medical Director, explains that it was established in Spring 2016 and attracted 260 expressions of interest. Now, 26 Doctors are working in 16 Practices in the region.
The fully-qualified GPs have come from seven EU countries: France, Spain, Italy, Poland, Romania, Lithuania and Croatia, having gone trough eligibility language assessment and face-to-face interviews with Practices.
To meet all the regulatory requirements for entry on to the national performers list, the Doctors in the Lincolnshire scheme first attended a 12-week residential intensive training programme at a campus in Poland. ‘This aimed to get candidates’ English language and knowledge and skills around basic NHS processes up to scratch,’ says Dr Sharrock. ‘They were given Bursaries to attend.’
Each Doctor completes a learning needs assessment, which feeds into their individualised personal development plan. They also have an individual clinical educational plan, which follows a similar blueprint to the MRCGP, covering areas including: clinical updates, screening and immunisation updates, medicines management and prescribing, regulatory aspects, primary care administration, unscheduled care and the role of allied health professionals.
In addition, the recruits have undertaken mandatory online training requirements, such as infection control, information governance and safeguarding
The GPs will be mentored by their recruiting practices, for which surgeries have been given a small amount of funding, Dr Sharrock adds.
MPs TAKE ON HUNT ABOUT ACCOUNTABLE CARE ORGANISATION ROLL-OUT. JUDICIAL REVIEW!
We expect this to be one of the most intense debates on the NHS for years.
25 January 2018
Instead of arguing it out with Sarah Wollaston’s Health Select Committee, Jeremy Hunt has wisely opted for a wider public consultation and it will mobilise all the national stakeholder groups, as well as local politicians, NHS campaigners and the general public. No doubt there will be petitions as well; 38 degrees and others portray this as surrogate privatisation.
Much, therefore, depends upon the Department of Health and Social Care ensuring a 100% quality process – or an Autumn Judicial Review, to coincide with the Party Conference season, will be the safest prediction of the year.
Article:Health and Social Care Secretary, Jeremy Hunt, has revealed that NHS England and the Government are likely to push back the creation of the first Accountable Care Organisations (ACOs) until a national consultation can be held on the issue.
In a letter to the Commons Health Select Committee, Hunt said the details of exactly how ACOs will work, including the contract terms involved, need to be made clear before more work is done.
The news comes in response to letter sent last week from Sarah Wollaston, Chair of the Committee, which urged the Health and Care secretary to delay the introduction of ACOs until the Committee had been able to hear evidence on the subject.
Wollaston said there had been “a great deal of concern” about the development of Accountable Care models, and that there needed to be a public forum to air these issues.
Hunt also revealed that some of the Legislation surrounding ACOs, which was due to be enacted in February, is likely to be delayed until the consultation can be completed.
In her letter, Wollaston explained that a consultation would be a chance to hear “both sides of the arguments” on the implementation of ACOs.
Responding, Hunt said that he expected NHS England’s national public consultation on the draft ACO contract, which will be released in Spring this year, would explain “what ACOs are and are not,” as well as covering the terms of the contract.
He added that some areas in England, which have already begun to establish Accountable Care could be “in a position to sign an ACO contract later in 2018.”
ACOs are part of an attempt by Central Government to improve the integration of care between the NHS, Local Authorities and other partners. It emphasises place and population rather than specific organisations or groups, and is hoped to improve some of the issues surrounding the link between health and social care.
The term ‘accountable care’ actually comes from the United States, where ACOs, under a slightly different format, were set up during President Obama’s health reforms.
Speaking to NHE earlier this month, Duncan Selbie, Public Health England (PHE) Chief Executive, explained the way Accountable Health will fit into the health system in the future, with reference to the way STPs will work within the NHS.
Article originally appeared on National Health Executive
----------------------------------------------------------------------------------------------------------------------------------- JUDICIAL REVIEW
Accountable Care Organisations and the USA Medicare model of healthcare, must not be allowed to be seen as 'the norm' and become entrenched in the NHS.
This is a huge public interest case. It affects all of us. Keep the date of the Judicial Review in your diary: Tuesday 24th April, Leeds Combined Court Centre - 10am.
We expect this to be one of the most intense debates on the NHS for years.
25 January 2018
Instead of arguing it out with Sarah Wollaston’s Health Select Committee, Jeremy Hunt has wisely opted for a wider public consultation and it will mobilise all the national stakeholder groups, as well as local politicians, NHS campaigners and the general public. No doubt there will be petitions as well; 38 degrees and others portray this as surrogate privatisation.
Much, therefore, depends upon the Department of Health and Social Care ensuring a 100% quality process – or an Autumn Judicial Review, to coincide with the Party Conference season, will be the safest prediction of the year.
Article:Health and Social Care Secretary, Jeremy Hunt, has revealed that NHS England and the Government are likely to push back the creation of the first Accountable Care Organisations (ACOs) until a national consultation can be held on the issue.
In a letter to the Commons Health Select Committee, Hunt said the details of exactly how ACOs will work, including the contract terms involved, need to be made clear before more work is done.
The news comes in response to letter sent last week from Sarah Wollaston, Chair of the Committee, which urged the Health and Care secretary to delay the introduction of ACOs until the Committee had been able to hear evidence on the subject.
Wollaston said there had been “a great deal of concern” about the development of Accountable Care models, and that there needed to be a public forum to air these issues.
Hunt also revealed that some of the Legislation surrounding ACOs, which was due to be enacted in February, is likely to be delayed until the consultation can be completed.
In her letter, Wollaston explained that a consultation would be a chance to hear “both sides of the arguments” on the implementation of ACOs.
Responding, Hunt said that he expected NHS England’s national public consultation on the draft ACO contract, which will be released in Spring this year, would explain “what ACOs are and are not,” as well as covering the terms of the contract.
He added that some areas in England, which have already begun to establish Accountable Care could be “in a position to sign an ACO contract later in 2018.”
ACOs are part of an attempt by Central Government to improve the integration of care between the NHS, Local Authorities and other partners. It emphasises place and population rather than specific organisations or groups, and is hoped to improve some of the issues surrounding the link between health and social care.
The term ‘accountable care’ actually comes from the United States, where ACOs, under a slightly different format, were set up during President Obama’s health reforms.
Speaking to NHE earlier this month, Duncan Selbie, Public Health England (PHE) Chief Executive, explained the way Accountable Health will fit into the health system in the future, with reference to the way STPs will work within the NHS.
Article originally appeared on National Health Executive
----------------------------------------------------------------------------------------------------------------------------------- JUDICIAL REVIEW
Accountable Care Organisations and the USA Medicare model of healthcare, must not be allowed to be seen as 'the norm' and become entrenched in the NHS.
This is a huge public interest case. It affects all of us. Keep the date of the Judicial Review in your diary: Tuesday 24th April, Leeds Combined Court Centre - 10am.
|
PUBLIC ACCOUNTS COMMITTEE REPORT INTO CONTINUING HEALTHCARE
56 pages NHS continuing healthcare funding intended to help some of the most vulnerable people in society is not reaching people who need it. That’s one of the conclusions of the latest parliamentary report which describes a complex process beset with delays and poor-quality assessments. https://publications.parliament.uk/pa/cm201719/cmselect/cmpubacc/455/455.pdf |
NHS England began the process of allocating the £45m of funding for online consultations to CCGs in November last year.
Practices are not required to undertake online consultations, but NHS England has said it hopes the majority will benefit from the fund over the three-year period it is available.
In the survey of 231 GP partners, 58% said that their practice did not currently offer online consultations and was not interested in doing so. Some 10% of partners said that their practice already provided the service to patients. The remaining 32% said that their practice did not currently provide online consultations, but was interested in doing so in the future.
GPs say:
Practices are not required to undertake online consultations, but NHS England has said it hopes the majority will benefit from the fund over the three-year period it is available.
In the survey of 231 GP partners, 58% said that their practice did not currently offer online consultations and was not interested in doing so. Some 10% of partners said that their practice already provided the service to patients. The remaining 32% said that their practice did not currently provide online consultations, but was interested in doing so in the future.
GPs say:
- Dangerous for all but simplest requests.
- Practice currently providing online consultations said: 'We will be looking to withdraw from the service as it has increased, rather than decreased, our workload.'
- Increased the workload as these patients nearly always need a phone consultation or a face-to-face appointment.'
- More positive , 'better access for patients – it's not exactly time saving but it does make triage easier.
CCG ASSESSMENTS
The CCG 360-degree stakeholder survey 2017/18 will be conducted by Ipsos MORI on behalf of NHS England from 15 January to 23 February 2018.
The survey directly contributes to the annual assessment of CCGs under the CCG improvement and assessment framework and provides valuable feedback and learning opportunities for CCGs, supporting them to strengthen their work with stakeholders to improve services and health outcomes for their local populations.
CCGs should take this opportunity to maximise their survey response rates by encouraging their nominated stakeholders to complete the survey and where appropriate explaining to them how they have used previous survey findings for improvement purposes.
The CCG 360-degree stakeholder survey 2017/18 will be conducted by Ipsos MORI on behalf of NHS England from 15 January to 23 February 2018.
The survey directly contributes to the annual assessment of CCGs under the CCG improvement and assessment framework and provides valuable feedback and learning opportunities for CCGs, supporting them to strengthen their work with stakeholders to improve services and health outcomes for their local populations.
CCGs should take this opportunity to maximise their survey response rates by encouraging their nominated stakeholders to complete the survey and where appropriate explaining to them how they have used previous survey findings for improvement purposes.
RESHUFFLE - MINISTERIAL TEAM
Philip Dunne, formally Minister of State for Health, responsible for patient involvement etc, is no longer on the Ministerial Health Team.
Caroline Dinenage was appointed on 9 January 2018. Caroline was Parliamentary Under Secretary of State at the Department for Work and Pensions from June 2017 to January 2018. She was Parliamentary Under Secretary of State for Women, Equalities and Early Years at the Department for Education from July 2016 to June 2017.
“Ministerial responsibilities will be confirmed in due course.” – D of H and SC
Philip Dunne, formally Minister of State for Health, responsible for patient involvement etc, is no longer on the Ministerial Health Team.
Caroline Dinenage was appointed on 9 January 2018. Caroline was Parliamentary Under Secretary of State at the Department for Work and Pensions from June 2017 to January 2018. She was Parliamentary Under Secretary of State for Women, Equalities and Early Years at the Department for Education from July 2016 to June 2017.
“Ministerial responsibilities will be confirmed in due course.” – D of H and SC
CQC CHIEF TO GO IN THE SUMMER
Sir David Behan has announced his intention to step down as Chief Executive of the Care Quality Commission in the Summer.
Sir David joined in 2012, at a time of huge controversy about the behaviour of and standards at the regulator. It has made substantial changes to how it works under his leadership, many in response to the Francis inquiry into events at Mid Staffordshire Foundation Trust.
Sir David Behan has announced his intention to step down as Chief Executive of the Care Quality Commission in the Summer.
Sir David joined in 2012, at a time of huge controversy about the behaviour of and standards at the regulator. It has made substantial changes to how it works under his leadership, many in response to the Francis inquiry into events at Mid Staffordshire Foundation Trust.
2017 - 2019 NHS STANDARD CONTRACT: UPDATED JANUARY 2018
The NHS Standard Contract is mandated by NHS England for use by commissioners for all contracts for healthcare services other than primary care.
Where Commissioners are placing new contracts with providers, they must now use these updated versions of the relevant Contract with immediate effect.
A summary of the changes we have made to the Contracts can be found in section 3 of the NHS Standard Contract Technical Guidance. Details of the changes can be found in the comparison documents below.
The full –length NHS Standard Contract 2017/18-2018/19 (January 2018 edition) comprises three parts:
The NHS shorter-form Contract 2017/18-2018/19 (January 2018 edition) also comprises three parts:
If you have a query on the NHS Standard Contracts, please email: [email protected].
If you would like to be added to our stakeholder list to receive updates on the NHS Standard Contracts, please email your contact details to: [email protected].
To read more, go to: https://www.england.nhs.uk/nhs-standard-contract/17-19-updated/
The NHS Standard Contract is mandated by NHS England for use by commissioners for all contracts for healthcare services other than primary care.
Where Commissioners are placing new contracts with providers, they must now use these updated versions of the relevant Contract with immediate effect.
A summary of the changes we have made to the Contracts can be found in section 3 of the NHS Standard Contract Technical Guidance. Details of the changes can be found in the comparison documents below.
The full –length NHS Standard Contract 2017/18-2018/19 (January 2018 edition) comprises three parts:
- Particulars - Service Conditions - General Conditions
The NHS shorter-form Contract 2017/18-2018/19 (January 2018 edition) also comprises three parts:
- Particulars - Service Conditions - General Conditions
If you have a query on the NHS Standard Contracts, please email: [email protected].
If you would like to be added to our stakeholder list to receive updates on the NHS Standard Contracts, please email your contact details to: [email protected].
To read more, go to: https://www.england.nhs.uk/nhs-standard-contract/17-19-updated/
NEW NON-EXECUTIVES JOIN THE CQC BOARD
08 January 2018
Three new Non-Executive Board Members have been appointed to the Care Quality Commission.
Sir John Oldham joins the regulator’s Board and will bring expertise in system integration and healthcare productivity. In 2013, he led an independent commission on whole person care for the Labour party when Ed Miliband was leader, which helped inform the party’s Health and Social Care Policies. He was also National Clinical Lead for Quality and Productivity at the Department of Health, and a member of NHS England’s National Quality Board.
Sir John retains his position as Adjunct Professor at the Institute of Global Health at Imperial College.
Liz Sayce also joins the Non-Executive Board. She has a history of championing the rights of disabled people, including lobbying for the introduction of Disability Discrimination Act in 1995 and heading up a controversial government review six years ago into disability employment. She was chief executive of Disability Rights UK until May 2017, and remains a member of the government’s Social Security Advisory Committee.
The third appointment is Mark Saxton. He has a background in workforce and pay, chairing committees on these issues when he was a Non-Executive Director of Yeovil District Hospital Foundation Trust. Prior to that, he held senior positions in HR and general management at FTSE, and NYSE listed companies internationally and in the UK.
Ms Sayce and Sir John took up their roles at the start of the year. Mr Saxton will join on 01 March.
The new Non-Executive Directors are replacing Michael Mire, Kay Sheldon and Jennifer Dixon who left last year.
CQC Chair, Peter Wyman said: “Our three new Non-Executive Directors bring a wealth of diverse experience which complements the expertise we already have, and will help us deliver our strategy.”
08 January 2018
Three new Non-Executive Board Members have been appointed to the Care Quality Commission.
Sir John Oldham joins the regulator’s Board and will bring expertise in system integration and healthcare productivity. In 2013, he led an independent commission on whole person care for the Labour party when Ed Miliband was leader, which helped inform the party’s Health and Social Care Policies. He was also National Clinical Lead for Quality and Productivity at the Department of Health, and a member of NHS England’s National Quality Board.
Sir John retains his position as Adjunct Professor at the Institute of Global Health at Imperial College.
Liz Sayce also joins the Non-Executive Board. She has a history of championing the rights of disabled people, including lobbying for the introduction of Disability Discrimination Act in 1995 and heading up a controversial government review six years ago into disability employment. She was chief executive of Disability Rights UK until May 2017, and remains a member of the government’s Social Security Advisory Committee.
The third appointment is Mark Saxton. He has a background in workforce and pay, chairing committees on these issues when he was a Non-Executive Director of Yeovil District Hospital Foundation Trust. Prior to that, he held senior positions in HR and general management at FTSE, and NYSE listed companies internationally and in the UK.
Ms Sayce and Sir John took up their roles at the start of the year. Mr Saxton will join on 01 March.
The new Non-Executive Directors are replacing Michael Mire, Kay Sheldon and Jennifer Dixon who left last year.
CQC Chair, Peter Wyman said: “Our three new Non-Executive Directors bring a wealth of diverse experience which complements the expertise we already have, and will help us deliver our strategy.”