NEWS - OCTOBER 2018
|
FUNDING - LOCAL HEALTHWATCH -2018 ... 17 pages
Across England, there are 152 Local Healthwatch services. Their statutory role is to find out what people want from health and care and to share these views with those running services to help make them better. Local Healthwatch also provides people with information and advice about services. Check table at the end, for state of your area’s LHW cash! |
ROBERT FRANCIS ATTACKS 'PERILOUS STATE' OF LOCAL HEALTHWATCH FUNDING
01 November 2018 ... 2 pages
Funding of Local Healthwatch services has been plunged into a “perilous state” and their effectiveness is starting to be impaired, Sir Robert Francis has warned.
In a letter to health and social care secretary Matt Hancock, the chairman of the Mid Staffordshire Public Inquiry warned the numbers of full time staff employed by Healthwatch had crashed by 22 per cent in two years, while this year’s funding for some local areas had been slashed by 50 per cent.
01 November 2018 ... 2 pages
Funding of Local Healthwatch services has been plunged into a “perilous state” and their effectiveness is starting to be impaired, Sir Robert Francis has warned.
In a letter to health and social care secretary Matt Hancock, the chairman of the Mid Staffordshire Public Inquiry warned the numbers of full time staff employed by Healthwatch had crashed by 22 per cent in two years, while this year’s funding for some local areas had been slashed by 50 per cent.
ICPs and LOCAL HEALTHWATCH ... Hansard Source (Citation: HC Deb, 31 October 2018, cW)
George Howarth Labour, Knowsley
To ask the Secretary of State for Health and Social Care, what plans he has in place to enable Integrated Care Providers to work with local Healthwatch groups.
Stephen Barclay Minister of State (Department of Health and Social Care)NHS England launched a 12 week public consultation on the proposed contracting arrangements for integrated care providers on 3 August 2018 which concluded on 26 October. More information is available at the following link:
https://www.engage.england.nhs.uk/consultation/proposed-contracting-arrangements-for-icps/
NHS England will publish a response to the consultation following full consideration of responses and feedback. The consultation will also consider how integrated care providers cooperate with Local Healthwatch.
George Howarth Labour, Knowsley
To ask the Secretary of State for Health and Social Care, what plans he has in place to enable Integrated Care Providers to work with local Healthwatch groups.
Stephen Barclay Minister of State (Department of Health and Social Care)NHS England launched a 12 week public consultation on the proposed contracting arrangements for integrated care providers on 3 August 2018 which concluded on 26 October. More information is available at the following link:
https://www.engage.england.nhs.uk/consultation/proposed-contracting-arrangements-for-icps/
NHS England will publish a response to the consultation following full consideration of responses and feedback. The consultation will also consider how integrated care providers cooperate with Local Healthwatch.
CQC DATA TO BE OPEN TO THE PUBLIC ... 1 page
The public will be granted increased access to data held by the Care Quality Commission about the quality of care provided by NHS organisations and GPs, the regulator’s new Chief Executive has pledged.
Speaking to MPs this afternoon, the watchdog’s new Chief Executive, Ian Trenholm, told the Health and Social Care Select Committee he wants to open up the CQC’s data streams.
The public will be granted increased access to data held by the Care Quality Commission about the quality of care provided by NHS organisations and GPs, the regulator’s new Chief Executive has pledged.
Speaking to MPs this afternoon, the watchdog’s new Chief Executive, Ian Trenholm, told the Health and Social Care Select Committee he wants to open up the CQC’s data streams.
WANT AN ICS? THEN YOU WILL NEED SOME OF THESE ...
Primary Care Networks (PCNs) are at the heart of the developing integrated care systems starting to spring up across England.
In many areas NHS England’s desire to see GP practices working together in PCNs that integrate community healthcare at scale is now backed by resources.
PCNs are groups of GP practices working with a range of statutory and voluntary sector organisations to deliver integrated community health and wellbeing. NHS England’s preferred population size for PCNs is 30,000-50,000. A consensus is emerging that this is the most appropriate range for delivering primary care at scale without losing the local feel of NHS services.
The thinking behind PCNs is that they should promote collaborative working between practices and their partners while shaping collective solutions to local problems.
While many practices – including those led by some of the more effective and forward-looking GP federations – have travelled a long way down the PCN path, some are still groping their way towards the development of a meaningful PCN.
Whatever stage your practice has reached, the building blocks that will create an effective PCN provide you, neighbouring practices and other partners with the chance to take stock of how you meet your patients’ needs, ensure your practice is sustainable for the future, help your practice consider workforce challenges and ensure best use of NHS resources.
The building blocks for working together include identifying leaders, vision and purpose, asking who you want to work with locally and why, identifying workforce and capacity requirements and coming up with a credible business plan.
PCNs might what to consider how they support the local extended hours offer and other locally commissioned services.
It means working with local practices and other providers to evaluate what additional services can be delivered in the community – and the skill mix needed, both in your practice and the wider network. What role, for example, will paramedics and clinical pharmacists play and who will employ them?
Practices are having to consider what partners – including voluntary sector organisations and community health providers – they can work with most effectively.
And because this process must be driven by local leaders, some areas with relatively well-established PCN boards need to review their business strategy and consider how to improve their communications with member practices and local stakeholders.
Even the most advanced PCN can benefit from this opportunity to pause and reflect on their business objectives and business plan.
NHS England sees the development of PCNs as a priority – and is funding some of that work.
Primary Care Networks (PCNs) are at the heart of the developing integrated care systems starting to spring up across England.
In many areas NHS England’s desire to see GP practices working together in PCNs that integrate community healthcare at scale is now backed by resources.
PCNs are groups of GP practices working with a range of statutory and voluntary sector organisations to deliver integrated community health and wellbeing. NHS England’s preferred population size for PCNs is 30,000-50,000. A consensus is emerging that this is the most appropriate range for delivering primary care at scale without losing the local feel of NHS services.
The thinking behind PCNs is that they should promote collaborative working between practices and their partners while shaping collective solutions to local problems.
While many practices – including those led by some of the more effective and forward-looking GP federations – have travelled a long way down the PCN path, some are still groping their way towards the development of a meaningful PCN.
Whatever stage your practice has reached, the building blocks that will create an effective PCN provide you, neighbouring practices and other partners with the chance to take stock of how you meet your patients’ needs, ensure your practice is sustainable for the future, help your practice consider workforce challenges and ensure best use of NHS resources.
The building blocks for working together include identifying leaders, vision and purpose, asking who you want to work with locally and why, identifying workforce and capacity requirements and coming up with a credible business plan.
PCNs might what to consider how they support the local extended hours offer and other locally commissioned services.
It means working with local practices and other providers to evaluate what additional services can be delivered in the community – and the skill mix needed, both in your practice and the wider network. What role, for example, will paramedics and clinical pharmacists play and who will employ them?
Practices are having to consider what partners – including voluntary sector organisations and community health providers – they can work with most effectively.
And because this process must be driven by local leaders, some areas with relatively well-established PCN boards need to review their business strategy and consider how to improve their communications with member practices and local stakeholders.
Even the most advanced PCN can benefit from this opportunity to pause and reflect on their business objectives and business plan.
NHS England sees the development of PCNs as a priority – and is funding some of that work.
|
FEEDBACK IN DISTRESSING SITUATIONS - 26 October 2018
https://www.england.nhs.uk/wp-content/uploads/2016/09/bitesize-guide-seeking-feedback-in-distressing-or-highly-emotional-distressing-situations.pdf Asking patients who have gone through distressing experiences for feedback can be challenge. NHS England has published a brief guide to seeking feedback in these situations. It is the latest in a set of guides aimed at commissioners and providers to help them to record patients’ experiences of NHS services. https://www.england.nhs.uk/wp-content/uploads/2016/09/bite-size-guide-whats-already-available-v2.pdf |
|
GPS 'ON-LINE SERVICES' FOR PATIENTS
The GP online services team developed this toolkit to support GPs to promote online services to their patients and encourage them to register for GP online services. The aim of this toolkit is to help GPs to: • Promote GP online services to the public • Increase patient awareness so that they are able to use GP online services |
|
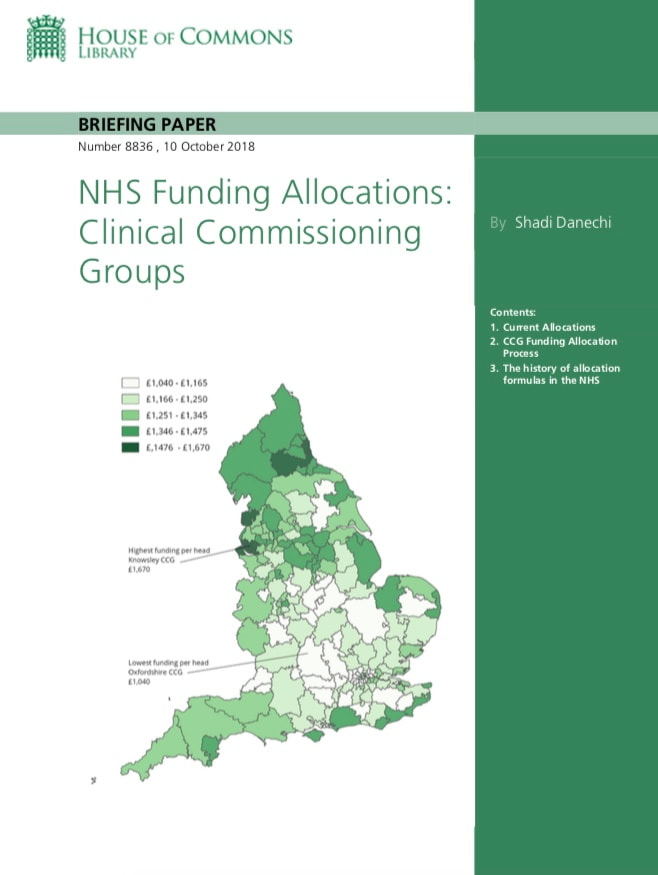
CCGs - WHO GETS WHAT
In 2018/19 NHS England distributed a total of £74.2 billion across 195 CCGs in England. The overall funding equates to £1,254 per registered patient in England. Funding per head increased in real terms between 2013/14 and 2018/19. The average annual increase from 2013/14 to 2018/19 was 2%. The formula used to distribute funding means that CCGs with elderly populations, in urban areas, or in more deprived areas, tend to have higher allocations than they would under a simple population-based formula. The highest allocation per patient in 2018/19 is Knowsley CCG in Merseyside (£1,645), the lowest CCG allocation per patient is Oxfordshire CCG (£1,040). All of the 10 highest allocations per patient are CCGs in the North East and North West of England. |
OPTING OUT OF SHARING OUR RECORDS - Poor uptake of new scheme to give patients control of confidential records
A new national system to give NHS patients control over sharing their confidential health records has been used by less than 5,000 people, leading to accusations that it has been poorly publicised. The national data opt-out went live on 25 May this year and gave every NHS patient the ability to opt out of sharing their personal health data beyond direct care. At the time, NHS England said there would be a public campaign focusing to “ensure messages are reaching the public in a clear and accessible way”.
However, NHS Digital figures show that in the four months to 1 October, only 2,185 people used the national opt- out to prevent sharing of their confidential health records. That number dropped sharply in the past two months, with only 306 people opting out in September. More people used the system to opt in instead, with 2807 saying they now wanted to share more information after previously saying they did not.
The new system also remains far less popular than the old “type-2” opt out, set up in 2014 as part of Care.data and controlled directly by a patient’s GP. Despite more than 26,000 patients lodging a “type-2” opt out with their GP in the three months to 1 September, that system will close today. A total of 1.5 million patients have registered a type-2 objection since 2014 moving to the new system.
NHS England had written to 1.5 million patients being shifted onto the new national system, but there has been little broader publicity. What about the other 98 per cent of people out there? The new system still had shortcomings, including making it more difficult for parents to opt out on behalf of their children. However, King’s
Fund researcher Harry Evans said the low levels of opt outs under the new system was positive. Of more concern was continuing high level opt-outs through patients’ GPs, which threatened service planning and research. “Now the national bodies have implemented the national data opt-out, they should make it their mission to investigate why people are continuing to opt out via their GP practices, even when a national, simple and standardised opt out option exists.”
In 2014, NHS England came under heavy criticism for its lacklustre publicity campaign for the Care.data patient record sharing scheme in 2014. The scheme was eventually closed in 2016. The new national opt out is viewed by NHS national leaders as critical to rebuilding public trust in data sharing but there is also concern that too many
patients opting out could compromise the quality of data for research and planning. A Department of Health and Social Care spokesman said efforts to inform patients about the opt out had included advertisements in most national newspapers, regional radio stations and leaflets and posters distributed for display in hospitals, GP practices and other care settings.
Tim Magor, National Data Opt-out Programme Head at NHS Digital, said the old system had been in place since 2014 and it was expected to take time for people to switch. “The national data opt out gives patients a more direct choice about how their information can be used and enables them to review that choice and change it whenever they choose, without placing an unacceptable additional burden on GPs. “As type-2s are fully retired on 11 October, use of the national data opt out service may increase as we continue to make patients aware of how they can make choices about the use of their data.”
NHS patient opt-outs explained
A new national data opt-out was a key recommendation of National Data Guardian Dame Fiona Caldicott’s third report, published in July 2016.
The report was focused on resolving years of controversy over how much patient identifiable NHS data is shared without their explicit consent, particularly for commercial research. Under the previous consent model set-up in 2014 as part of Care.data, patients could ask their GP to stop sharing their GP records with NHS Digital (known as a type-1 opt-out) or sharing any of their identifiable health records beyond NHS Digital (known as a type-2). Type-2 opt-outs were registered with a patient’s GP and applied by NHS Digital. The new opt-out was launched on 25 May this year, replacing the type-2 scheme with a single objection to any sharing of patient identifiable information for purposes beyond direct care. Unlike the previous scheme, every health and care organisation will be expected to honour these preferences by 2020-21.
The opt-out is currently honoured by NHS Digital and Public Health England. It is run directly by NHS Digital, rather than GPs, and run mostly online, although off-line options are available.
A new national system to give NHS patients control over sharing their confidential health records has been used by less than 5,000 people, leading to accusations that it has been poorly publicised. The national data opt-out went live on 25 May this year and gave every NHS patient the ability to opt out of sharing their personal health data beyond direct care. At the time, NHS England said there would be a public campaign focusing to “ensure messages are reaching the public in a clear and accessible way”.
However, NHS Digital figures show that in the four months to 1 October, only 2,185 people used the national opt- out to prevent sharing of their confidential health records. That number dropped sharply in the past two months, with only 306 people opting out in September. More people used the system to opt in instead, with 2807 saying they now wanted to share more information after previously saying they did not.
The new system also remains far less popular than the old “type-2” opt out, set up in 2014 as part of Care.data and controlled directly by a patient’s GP. Despite more than 26,000 patients lodging a “type-2” opt out with their GP in the three months to 1 September, that system will close today. A total of 1.5 million patients have registered a type-2 objection since 2014 moving to the new system.
NHS England had written to 1.5 million patients being shifted onto the new national system, but there has been little broader publicity. What about the other 98 per cent of people out there? The new system still had shortcomings, including making it more difficult for parents to opt out on behalf of their children. However, King’s
Fund researcher Harry Evans said the low levels of opt outs under the new system was positive. Of more concern was continuing high level opt-outs through patients’ GPs, which threatened service planning and research. “Now the national bodies have implemented the national data opt-out, they should make it their mission to investigate why people are continuing to opt out via their GP practices, even when a national, simple and standardised opt out option exists.”
In 2014, NHS England came under heavy criticism for its lacklustre publicity campaign for the Care.data patient record sharing scheme in 2014. The scheme was eventually closed in 2016. The new national opt out is viewed by NHS national leaders as critical to rebuilding public trust in data sharing but there is also concern that too many
patients opting out could compromise the quality of data for research and planning. A Department of Health and Social Care spokesman said efforts to inform patients about the opt out had included advertisements in most national newspapers, regional radio stations and leaflets and posters distributed for display in hospitals, GP practices and other care settings.
Tim Magor, National Data Opt-out Programme Head at NHS Digital, said the old system had been in place since 2014 and it was expected to take time for people to switch. “The national data opt out gives patients a more direct choice about how their information can be used and enables them to review that choice and change it whenever they choose, without placing an unacceptable additional burden on GPs. “As type-2s are fully retired on 11 October, use of the national data opt out service may increase as we continue to make patients aware of how they can make choices about the use of their data.”
NHS patient opt-outs explained
A new national data opt-out was a key recommendation of National Data Guardian Dame Fiona Caldicott’s third report, published in July 2016.
The report was focused on resolving years of controversy over how much patient identifiable NHS data is shared without their explicit consent, particularly for commercial research. Under the previous consent model set-up in 2014 as part of Care.data, patients could ask their GP to stop sharing their GP records with NHS Digital (known as a type-1 opt-out) or sharing any of their identifiable health records beyond NHS Digital (known as a type-2). Type-2 opt-outs were registered with a patient’s GP and applied by NHS Digital. The new opt-out was launched on 25 May this year, replacing the type-2 scheme with a single objection to any sharing of patient identifiable information for purposes beyond direct care. Unlike the previous scheme, every health and care organisation will be expected to honour these preferences by 2020-21.
The opt-out is currently honoured by NHS Digital and Public Health England. It is run directly by NHS Digital, rather than GPs, and run mostly online, although off-line options are available.
|
DIABETES - IN-PATIENT SERVICES
Diabetes UK has published a report that highlights the challenges facing diabetes inpatient services and shows what should be in place in all hospitals. |
|
IMPACT OF BREXIT ON THE NHS
This week the Department of Health and Social Care is set to instruct all trusts to carry out a detailed study of what impact the UK leaving the EU without a deal would have on their ability to purchase and maintain vital stock. The NHS spends £6bn every year on common goods, devices, and medical equipment. There are main suppliers to the NHS Supply Chain, the national system through which trusts can choose to buy products, but NHS trusts in total use tens of thousands of different suppliers for all the equipment needed to provide care to patients, and usage of NHS Supply Chain varies dramatically. |
Immediately after Brexit, existing UK regulations on procurement – which include EU directives – will continue to apply.The UK government wants to maintain the country’s membership of the World Trade Organisation’s Agreement on Government Procurement. This involves the UK opening up certain higher value public procurement opportunities to other countries, in exchange for their procurement markets being opened up in a similar way – according to a briefing published last month by the House of Commons Library.
|
NHS CONTINUING HEALCARE IN ENGLAND
By: Thomas Powell and Andrew Mackley - 27 September 2018 What is NHS Continuing Healthcare? - The National Framework - Dispute Resolution Refunds Guidance - Recent Developments - NHS Continuing Healthcare in other parts of the UK - Key Guidance Documents |
CQC CHIEF INSPECTOR QUITS TO LEAD NURSING WATCHDOG - 04 October 2018
The Care Quality Commission Chief Inspector of Adult Social Care, Andrea Sutcliffe, has been appointed the new Chief Executive of the Nursing and Midwifery Council.
Ms Sutcliffe, who joined the CQC in October 2013, will take on the role at the nursing watchdog in January 2019.
She replaces former NMC Chief, Jackie Smith, who resigned from the NMC in May, a time when it was heavily criticised for its handling of the Morecambe Bay maternity care scandal.
Andrea Sutcliffe stepped up as acting Chief Executive at the CQC following the departure of Sir David Behan earlier this year, before its new Chief joined. She has become known for championing what she called the “Mum Test” in regulation social care providers to ensure CQC was focused on what matters to people using services.
CQC Chair, Peter Wyman, said: “To say that Andrea made the role her own is an understatement – she is the first person to hold this role and in it, she has used her passion and commitment to make a real difference to people’s
care. She has championed people who use adult social care, called out poor care and celebrated good care. The phrase she coined, the ‘Mum Test’: is this care good enough for your mum? – really spoke to people as a meaningful assessment of quality that was also very personal. She will be much missed but I congratulate the Nursing and Midwifery Council on an outstanding appointment.”
Among other issues raised during her time as Chief Inspector, she has highlighted the need to bolster the workforce, and the need for the NHS to pay more attention to its impact on care staffing.
The Care Quality Commission Chief Inspector of Adult Social Care, Andrea Sutcliffe, has been appointed the new Chief Executive of the Nursing and Midwifery Council.
Ms Sutcliffe, who joined the CQC in October 2013, will take on the role at the nursing watchdog in January 2019.
She replaces former NMC Chief, Jackie Smith, who resigned from the NMC in May, a time when it was heavily criticised for its handling of the Morecambe Bay maternity care scandal.
Andrea Sutcliffe stepped up as acting Chief Executive at the CQC following the departure of Sir David Behan earlier this year, before its new Chief joined. She has become known for championing what she called the “Mum Test” in regulation social care providers to ensure CQC was focused on what matters to people using services.
CQC Chair, Peter Wyman, said: “To say that Andrea made the role her own is an understatement – she is the first person to hold this role and in it, she has used her passion and commitment to make a real difference to people’s
care. She has championed people who use adult social care, called out poor care and celebrated good care. The phrase she coined, the ‘Mum Test’: is this care good enough for your mum? – really spoke to people as a meaningful assessment of quality that was also very personal. She will be much missed but I congratulate the Nursing and Midwifery Council on an outstanding appointment.”
Among other issues raised during her time as Chief Inspector, she has highlighted the need to bolster the workforce, and the need for the NHS to pay more attention to its impact on care staffing.
THIRD OF MPs DO NOT UNDERSTAND NEW CARE MODEL JARGON
The majority of MPs want the NHS to simplify its language with a third admitting they do not understand new care model jargon.
New research found that 30 per cent of MPs did not understand what an “integrated care system” is and 34 per cent what “accountable care systems” were.
Nearly a quarter of Parliamentarians quizzed said they did not feel “sufficiently well informed” to scrutinise healthcare in Parliament, with just over half saying they did.
More than three quarters of MPs surveyed agreed NHS organisations should “simplify their language and explain concepts more clearly to Parliamentarians”.
The research was based on a survey of 108 MPs earlier this month carried out by YouGov for MHP Communications.
The survey also found:
Head of MHP’s health practice Kate Pogson said better communication would ultimately lead to better care for patients. She added: “We ask a lot of our elected officials. The brief of an MP is vast, and too often policy proposals are hidden behind overly complex jargonistic phrasing.
“Our research demonstrates how this is impacting on policymaking, with barely half feeling able to scrutinise healthcare issues effectively in Parliament.
“This is a shared endeavour: all of us working in the sector have a responsibility to explain concepts clearly.” MHP’s survey also found Labour MPs said they had a better understanding of healthcare terminology than Conservative MPs.
Labour MPs were nearly three times more likely to say they understood the concept of “holistic care” compared to Conservative colleagues and were more familiar with integrated care.
Source: MHP Survey
- More than a third of MPs do not understand the term “accountable care systems”, survey finds
- Report finds Parliamentarians want NHS communications teams to “explain concepts more clearly”
- YouGov survey finds 38 per cent do not know what “sustainable care” means
The majority of MPs want the NHS to simplify its language with a third admitting they do not understand new care model jargon.
New research found that 30 per cent of MPs did not understand what an “integrated care system” is and 34 per cent what “accountable care systems” were.
Nearly a quarter of Parliamentarians quizzed said they did not feel “sufficiently well informed” to scrutinise healthcare in Parliament, with just over half saying they did.
More than three quarters of MPs surveyed agreed NHS organisations should “simplify their language and explain concepts more clearly to Parliamentarians”.
The research was based on a survey of 108 MPs earlier this month carried out by YouGov for MHP Communications.
The survey also found:
- 60 per cent MPs said the language used to describe current changes in the NHS was not simple or easy to understand, compared to just 12 per cent who did;
- Three quarters of MPs agree that the level of knowledge required to understand exactly how the NHS works is significant;
- 19 per cent did not understand the term “integrated care”;
- 25 per cent did not understand what “outcomes based healthcare” was;
- 38 per cent said they did not understand the phrase “sustainable care”; and
- 52 per cent of MPs did not understand what “system approaches” were.
Head of MHP’s health practice Kate Pogson said better communication would ultimately lead to better care for patients. She added: “We ask a lot of our elected officials. The brief of an MP is vast, and too often policy proposals are hidden behind overly complex jargonistic phrasing.
“Our research demonstrates how this is impacting on policymaking, with barely half feeling able to scrutinise healthcare issues effectively in Parliament.
“This is a shared endeavour: all of us working in the sector have a responsibility to explain concepts clearly.” MHP’s survey also found Labour MPs said they had a better understanding of healthcare terminology than Conservative MPs.
Labour MPs were nearly three times more likely to say they understood the concept of “holistic care” compared to Conservative colleagues and were more familiar with integrated care.
Source: MHP Survey
|
THE HEALTH AND SOCIAL CARE INTERFACE
Ministry of Housing, Communities and Local Government Department of Health and Social Care and NHS England In this Report, discussions of 16 challenges to the improved joint working between health and social care are presented. Setting the Scene - The case for improved working at the interface between health and social care - Financial challenges - Culture and structure - Our audit approach. |