NEWS - NOVEMBER / DECEMBER 2019
CONTRACT DIRECTED ENHANCED SERVICE (DES) - NATIONAL SERVICE SPECIFICATIONS 2020/2021
GP Contract framework, which will be delivered by Primary Care Networks (PCNs) - in collaboration with community services and other providers - from April 2020.
The GP Contract framework set out seven national service specifications that will be added to the Network Contract DES: five starting from April 2020, and a further two from April 2021.
The five services are:
• Structured Medication Reviews and Optimisation
• Enhanced Health in Care Homes (jointly with community services providers)
• Anticipatory Care (jointly with community services providers)
• Personalised Care
• Supporting Early Cancer Diagnosis.
GP Contract framework, which will be delivered by Primary Care Networks (PCNs) - in collaboration with community services and other providers - from April 2020.
The GP Contract framework set out seven national service specifications that will be added to the Network Contract DES: five starting from April 2020, and a further two from April 2021.
The five services are:
• Structured Medication Reviews and Optimisation
• Enhanced Health in Care Homes (jointly with community services providers)
• Anticipatory Care (jointly with community services providers)
• Personalised Care
• Supporting Early Cancer Diagnosis.
NHSX PROJECTS TEAM SHEDS FIVE MEMBERS IN ONE MONTH ...
NHSX is a joint agency across NHS England and Improvement and the Department of Health and Social Care, set up by Health and Social Care Secretary, Matt Hancock, and working on major digital transformation projectsWork , including within urgent and emergency care, will continue “where appropriate” — despite five members of the team leaving within one month, NHSX has confirmed.
Director of Digital Transformation for NHSX, Sam Shah, left the role after his contract ended at the end of October — just four months after the unit officially launched.
NHSX has now confirmed a further four contracted members of the same team left in the weeks following Dr Shah’s departure, which a spokesman said was due to their contracts ending. They were not asked to renew. The Digital Transformation Team is involved with dozens of projects, including the development of Digital Urgent and Emergency Care and Digital Eye Care. There were originally nine people in the Team.
NHSX said the remaining members of the team will pick up any on-going work “where appropriate”. However, it is unclear whether the positions will be filled.
An NHSX spokesman said the team’s staffing needs are now being reviewed “with the aim of driving value for money and reducing reliance on external contractors where appropriate”.
NHSX is a joint agency across NHS England and Improvement and the Department of Health and Social Care, set up by Health and Social Care Secretary, Matt Hancock, and working on major digital transformation projectsWork , including within urgent and emergency care, will continue “where appropriate” — despite five members of the team leaving within one month, NHSX has confirmed.
Director of Digital Transformation for NHSX, Sam Shah, left the role after his contract ended at the end of October — just four months after the unit officially launched.
NHSX has now confirmed a further four contracted members of the same team left in the weeks following Dr Shah’s departure, which a spokesman said was due to their contracts ending. They were not asked to renew. The Digital Transformation Team is involved with dozens of projects, including the development of Digital Urgent and Emergency Care and Digital Eye Care. There were originally nine people in the Team.
NHSX said the remaining members of the team will pick up any on-going work “where appropriate”. However, it is unclear whether the positions will be filled.
An NHSX spokesman said the team’s staffing needs are now being reviewed “with the aim of driving value for money and reducing reliance on external contractors where appropriate”.
|
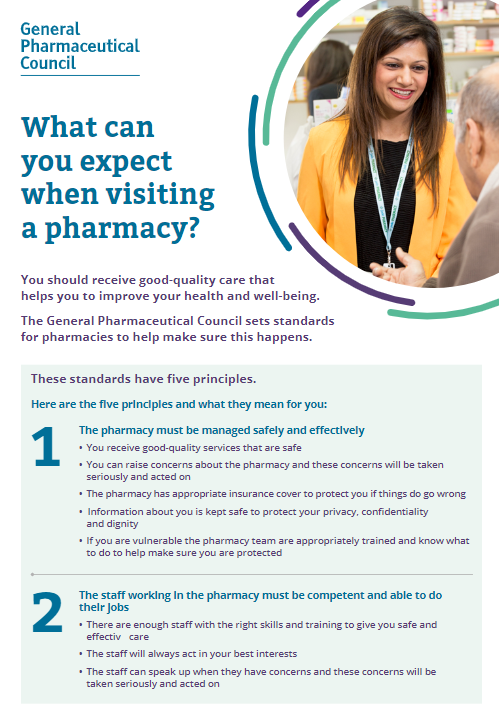
WHAT YOU CAN EXPECT WHEN VISITING A PHARMACY General Pharmaceutical Council - 3 pages You should receive good-quality care that helps you to improve your health and well-being. The General Pharmaceutical Council sets standards for pharmacies to help make sure this happens. |
|
SEARCHING LOCAL HEALTHWATCH REPORTS FOR ISSUES
Healthwatch has produced a tool that enables healthcare organisations to search nearly 3000 local Healthwatch publications for patient experience information. The reports contain more than 420,000 views of patients about their experience of the health and care system. |
|
PATIENT AND PUBLIC PARTICIPATION and CLINICAL COMMISSIONING GROUPS
NHS England has issued guidance on the patient and community engagement indicator in the NHS oversight framework 2019/20. The assessment framework remains the same as 2018/19 but there is now an option for CCGs merging from April 2020 to make a joint submission. Accountable officers have been sent an evidence template that needs to be completed by 1pm on Monday 10 February 2020. This guidance is for Clinical Commissioning Groups (CCGs) and NHS England. It supports staff to involve patients and the public in their work in a meaningful way to improve services, including giving clear advice on the legal duty to involve.
|
PHARMACY CONSULTING ROOMS ... 1 page
Pharmacies providing the Community Pharmacist Consultation Service (CPCS) must have IT equipment accessible within the Consultation Room to allow contemporaneous records of the CPCS consultations to be made within the CPCS IT system (PharmOutcomes or Sonar) from 1st April 2020.
This means that Pharmacists providing the service in the Consultation Room will need access to a desktop computer, laptop or tablet device with, as a minimum, access to the internet. This will enable access to the web-based CPCS IT systems, so records can be made while talking to the patient.
Pharmacies providing the Community Pharmacist Consultation Service (CPCS) must have IT equipment accessible within the Consultation Room to allow contemporaneous records of the CPCS consultations to be made within the CPCS IT system (PharmOutcomes or Sonar) from 1st April 2020.
This means that Pharmacists providing the service in the Consultation Room will need access to a desktop computer, laptop or tablet device with, as a minimum, access to the internet. This will enable access to the web-based CPCS IT systems, so records can be made while talking to the patient.
GP NUMBERS FALLING
According to NHS Digital figures, in September 2019 there were 28,315 FTE, fully-qualified GPs in England, compared with 28,654 a year earlier.
The figures show that the GP workforce has continued to stagnate despite repeated government promises to increase it.
[In September 2015, when then health and social care secretary Jeremy Hunt promised an extra 5,000 FTE GPs by 2020/21 - a promise eventually abandoned by his successor - there were 29,403 FTE fully qualified GPs - 1,088 (4%) more than the current figure.]
According to NHS Digital figures, in September 2019 there were 28,315 FTE, fully-qualified GPs in England, compared with 28,654 a year earlier.
The figures show that the GP workforce has continued to stagnate despite repeated government promises to increase it.
[In September 2015, when then health and social care secretary Jeremy Hunt promised an extra 5,000 FTE GPs by 2020/21 - a promise eventually abandoned by his successor - there were 29,403 FTE fully qualified GPs - 1,088 (4%) more than the current figure.]
PCNs PERMITTED TO PAY CHARITIES' MANAGEMENT COSTS
NHS England has made it easier for charities to be involved in primary care networks — by allowing ring-fenced budgets to be used to pay for third party management costs.
PCNs have been seeking to contract charities and other third sector organisations to supply thousands of Social Prescriber link workers. They are able to claim back 100 per cent of the salaries, national insurance and pension payments, from a ring-fenced national budget, to pay the organisations for the workers provided.
However, “nearly all” organisations supplying Social Prescribers have also passed additional management costs back to the PCNs, which were not covered by the central fund.
But now the national commissioner has decided PCNs can use some of this funding to contribute to these additional administrative costs, according to a letter to PCNs from NHSE.
PCNs can claim up to £34,113 for a Prescriber, and £2,400 of that can now be used to contribute to the additional employment costs. This money “is not in addition to the maximum reimbursable amount per role” and must be taken from the annual sum available for paying Social Prescribers.
It is hoped this will ease a major blockage on PCNs using the full extent of the additional roles reimbursement scheme before the end of March 2020 — a key NHS expectation for PCNs.
PCNs are meant to be hiring the Social Prescribers and Clinical Pharmacists in their first year. The additional workforce is seen as essential to alleviating GP workload while the requirements under the network contract get more onerous, starting with five new service specifications from April 2020.
Social Prescribing is a way for local agencies to refer people to a link worker. Link workers give people time, focusing on 'what matters to me' and taking a holistic approach to people's health and well-being. They connect people to community groups and statutory services for practical and emotional support.
NHS England has made it easier for charities to be involved in primary care networks — by allowing ring-fenced budgets to be used to pay for third party management costs.
PCNs have been seeking to contract charities and other third sector organisations to supply thousands of Social Prescriber link workers. They are able to claim back 100 per cent of the salaries, national insurance and pension payments, from a ring-fenced national budget, to pay the organisations for the workers provided.
However, “nearly all” organisations supplying Social Prescribers have also passed additional management costs back to the PCNs, which were not covered by the central fund.
But now the national commissioner has decided PCNs can use some of this funding to contribute to these additional administrative costs, according to a letter to PCNs from NHSE.
PCNs can claim up to £34,113 for a Prescriber, and £2,400 of that can now be used to contribute to the additional employment costs. This money “is not in addition to the maximum reimbursable amount per role” and must be taken from the annual sum available for paying Social Prescribers.
It is hoped this will ease a major blockage on PCNs using the full extent of the additional roles reimbursement scheme before the end of March 2020 — a key NHS expectation for PCNs.
PCNs are meant to be hiring the Social Prescribers and Clinical Pharmacists in their first year. The additional workforce is seen as essential to alleviating GP workload while the requirements under the network contract get more onerous, starting with five new service specifications from April 2020.
Social Prescribing is a way for local agencies to refer people to a link worker. Link workers give people time, focusing on 'what matters to me' and taking a holistic approach to people's health and well-being. They connect people to community groups and statutory services for practical and emotional support.
THE VOTE TO REMOVE HOME VISITS FROM GP CONTRACT
2 pages
LMCs in England have voted to remove home visits from the core GP contract, arguing that spiralling workload and workforce shortages mean the profession no longer has the capacity to deliver them.
2 pages
LMCs in England have voted to remove home visits from the core GP contract, arguing that spiralling workload and workforce shortages mean the profession no longer has the capacity to deliver them.
NHS PROPERTY - ISSUES ... Published 05 November 2019
17 pages
The Public Accounts Committee (PAC) says it is “unacceptable” that 70% of NHS Property Services' tenants do not have rental agreements.
NHS Property Services Limited has made progress in tackling some of the issues that it inherited when it was set up. However, it has struggled to get its tenants to sign rental agreements for the properties they occupy, and it is unacceptable that 70% of its tenants still do not have rental agreements in place. Without these agreements, it is very difficult to run an effective property management company and provide value for the NHS and taxpayers from the £3.8 billion estate that it was set up to manage. The lack of rental agreements has led to many bills being disputed, outstanding debt has almost tripled, to £576 million in March 2019, and £110 million of debt has been written off in the last five years.
The Department of Health & Social Care (the Department), NHS England and NHS Improvement and NHS Property Services have had six years to get a grip of this problem and have failed miserably. While we recognise that the situation is complex, and the provision of health services provided by tenants must continue uninterrupted by rental disputes, the whole system needs to work together far more effectively to find a solution which incentivises tenants to sign rental agreements and pay their bills promptly. We are concerned that the Department has yet to set out a course of action to address this problem, but instead is relying on others to find solutions without a clear timetable for achievement.
17 pages
The Public Accounts Committee (PAC) says it is “unacceptable” that 70% of NHS Property Services' tenants do not have rental agreements.
NHS Property Services Limited has made progress in tackling some of the issues that it inherited when it was set up. However, it has struggled to get its tenants to sign rental agreements for the properties they occupy, and it is unacceptable that 70% of its tenants still do not have rental agreements in place. Without these agreements, it is very difficult to run an effective property management company and provide value for the NHS and taxpayers from the £3.8 billion estate that it was set up to manage. The lack of rental agreements has led to many bills being disputed, outstanding debt has almost tripled, to £576 million in March 2019, and £110 million of debt has been written off in the last five years.
The Department of Health & Social Care (the Department), NHS England and NHS Improvement and NHS Property Services have had six years to get a grip of this problem and have failed miserably. While we recognise that the situation is complex, and the provision of health services provided by tenants must continue uninterrupted by rental disputes, the whole system needs to work together far more effectively to find a solution which incentivises tenants to sign rental agreements and pay their bills promptly. We are concerned that the Department has yet to set out a course of action to address this problem, but instead is relying on others to find solutions without a clear timetable for achievement.
NHS 111 REFERRAL FOR MINOR ILLNESSES AND URGENT MEDICINES SUPPLY
Almost three quarters (8,649) of the 11,600 Pharmacies in England have so far signed up to deliver the Community Pharmacy Consultation Service (CPCS), which went live last week (October 29), and sees Pharmacies receive £14 for each consultation they complete, following an NHS 111 referral for minor illnesses and urgent medicines supply.
Hull-based Pharmacy Manager, Laura Buckley, said her Pharmacy has handled four CPCS referrals so far; three being for an emergency supply and one for a minor illness.
Those needing an emergency supply believed the NHS 111 operator had sent a prescription to the Pharmacy, Ms Buckley claimed, which proved to be "time consuming" to then explain this was not the case, once she spoke to the patient.
Seeking a patient's permission to access their Summary Care Record (SCR) – a requirement under the CPCS – also proved time consuming, when it came to handling an emergency supply request for a care home patient.
"I was speaking to a representative and I asked if there was any reason why the lady couldn’t give me permission [to access her SCR]. [When I was transferred to her] at first, she said 'no'. After explaining the issue to her over the phone, I got permission to access her records, but that took about 35 minutes,” Ms Buckley explained.'
"According to the SCR, one medication had been stopped, so I then couldn’t emergency supply it," she added.
However, the minor ailment referral was easier to deal with and was potentially life-saving, she explained.
"The minor ailment was a skin rash. Prior to examination the rash could have potentially been shingles. Thankfully, in this case, I identified it as Contact Dermatitis and treated it with an over-the-counter product."
Almost three quarters (8,649) of the 11,600 Pharmacies in England have so far signed up to deliver the Community Pharmacy Consultation Service (CPCS), which went live last week (October 29), and sees Pharmacies receive £14 for each consultation they complete, following an NHS 111 referral for minor illnesses and urgent medicines supply.
Hull-based Pharmacy Manager, Laura Buckley, said her Pharmacy has handled four CPCS referrals so far; three being for an emergency supply and one for a minor illness.
Those needing an emergency supply believed the NHS 111 operator had sent a prescription to the Pharmacy, Ms Buckley claimed, which proved to be "time consuming" to then explain this was not the case, once she spoke to the patient.
Seeking a patient's permission to access their Summary Care Record (SCR) – a requirement under the CPCS – also proved time consuming, when it came to handling an emergency supply request for a care home patient.
"I was speaking to a representative and I asked if there was any reason why the lady couldn’t give me permission [to access her SCR]. [When I was transferred to her] at first, she said 'no'. After explaining the issue to her over the phone, I got permission to access her records, but that took about 35 minutes,” Ms Buckley explained.'
"According to the SCR, one medication had been stopped, so I then couldn’t emergency supply it," she added.
However, the minor ailment referral was easier to deal with and was potentially life-saving, she explained.
"The minor ailment was a skin rash. Prior to examination the rash could have potentially been shingles. Thankfully, in this case, I identified it as Contact Dermatitis and treated it with an over-the-counter product."
COMMUNITY PHARMACIST CONSULTATION SERVICE (CPCS)
The NHS Community Pharmacist Consultation Service (CPCS) has launched today (29th October), marking a significant moment for Community Pharmacy.
This new service enables NHS 111 to refer patients to Community Pharmacies when they have a minor illness or need an ’emergency supply’ of a medicine that they have previously been prescribed. The aim is to help relieve pressure on the wider NHS and speed up patient access to treatment by making use of Pharmacists’ core knowledge and skills.
The service is a key component of the five-year Community Pharmacy Contractual Framework (CPCF) settlement which came fully into effect this month.
Whilst referrals are currently only available via NHS 111, referrals from other settings, such as GP practices, are being piloted and are expected to be rolled out in the near future.
NB --- not all pharmacies are signed up to this yet.
The NHS Community Pharmacist Consultation Service (CPCS) has launched today (29th October), marking a significant moment for Community Pharmacy.
This new service enables NHS 111 to refer patients to Community Pharmacies when they have a minor illness or need an ’emergency supply’ of a medicine that they have previously been prescribed. The aim is to help relieve pressure on the wider NHS and speed up patient access to treatment by making use of Pharmacists’ core knowledge and skills.
The service is a key component of the five-year Community Pharmacy Contractual Framework (CPCF) settlement which came fully into effect this month.
Whilst referrals are currently only available via NHS 111, referrals from other settings, such as GP practices, are being piloted and are expected to be rolled out in the near future.
NB --- not all pharmacies are signed up to this yet.