NEWS - FEBRUARY 2014
MEDICAL RECORDS SHARE PLAN DELAYED
19 February 2014 - The Press Association
Controversial plans to share medical records will be delayed until later this year “to allow more time to build understanding of the benefits of using the information”, health officials have said.
Pressure has been mounting on NHS England, the body behind the scheme, after doctors leaders said patients need to know how their data will be used outside the health service.
Both the British Medical Association and the Royal College of GPs have warned that patients are being kept in the dark about the plans.
NHS England said the rollout of the scheme, that was due to take place in April, will now happen later this year.
A spokesman said: “To ensure that the concerns of the BMA, RCGP, Healthwatch and other groups are met, NHS England will begin collecting data from GP surgeries in the Autumn, instead of April, to allow more time to build understanding of the benefits of using the information, what safeguards are in place, and how people can opt out if they choose to.”
Patients, doctors and other professional organisations, have raised concerns that they have not been given enough time to learn about the project.
19 February 2014 - The Press Association
Controversial plans to share medical records will be delayed until later this year “to allow more time to build understanding of the benefits of using the information”, health officials have said.
Pressure has been mounting on NHS England, the body behind the scheme, after doctors leaders said patients need to know how their data will be used outside the health service.
Both the British Medical Association and the Royal College of GPs have warned that patients are being kept in the dark about the plans.
NHS England said the rollout of the scheme, that was due to take place in April, will now happen later this year.
A spokesman said: “To ensure that the concerns of the BMA, RCGP, Healthwatch and other groups are met, NHS England will begin collecting data from GP surgeries in the Autumn, instead of April, to allow more time to build understanding of the benefits of using the information, what safeguards are in place, and how people can opt out if they choose to.”
Patients, doctors and other professional organisations, have raised concerns that they have not been given enough time to learn about the project.
|
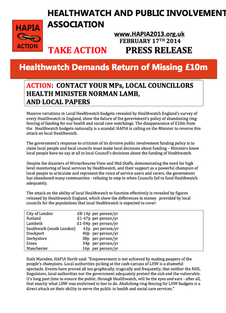
** PRESS RELEASE **
___________________________________ TAKE ACTION - HEALTHWATCH DEMANDS RETURN OF MISSING £10M HAPIA - 3 pages - 17 February 2014 ___________________________________ Click here for the HSJ Report 2 pages - 13 February 2014 |
HEALTH AND WELLBEING BOARDS
Diana Johnson (Shadow Minister (Home Affairs); Kingston upon Hull North, Labour) - to ask the Secretary of State for Health how many Health and Wellbeing Boards include representatives of the criminal justice community.
Norman Lamb (The Minister of State, Department of Health; North Norfolk, Liberal Democrat)
Health and wellbeing boards have the flexibility to determine their own membership in a way that best meets the needs of their local communities.
The Health and Social Care Act 2012 sets a core membership that boards must include:
There is no requirement, therefore, on Boards to include membership from the criminal justice community, and the Department does not keep information on the membership of individual boards.
However, membership is not the only way to engage with the work of Boards. We expect Boards will want to ensure that they have wider mechanisms in place to draw on the expertise of other groups when developing their Joint Health and Wellbeing Strategies and the Joint Strategic Needs Assessments on which they are based.
Diana Johnson (Shadow Minister (Home Affairs); Kingston upon Hull North, Labour) - to ask the Secretary of State for Health how many Health and Wellbeing Boards include representatives of the criminal justice community.
Norman Lamb (The Minister of State, Department of Health; North Norfolk, Liberal Democrat)
Health and wellbeing boards have the flexibility to determine their own membership in a way that best meets the needs of their local communities.
The Health and Social Care Act 2012 sets a core membership that boards must include:
- At least one Councillor from the Local Authority;
- The Director of Adult Social Services;
- The Director of Children's Services;
- The Director of Public Health;
- A representative of the Local Healthwatch;
- A representative of each relevant local Clinical Commissioning Group.
There is no requirement, therefore, on Boards to include membership from the criminal justice community, and the Department does not keep information on the membership of individual boards.
However, membership is not the only way to engage with the work of Boards. We expect Boards will want to ensure that they have wider mechanisms in place to draw on the expertise of other groups when developing their Joint Health and Wellbeing Strategies and the Joint Strategic Needs Assessments on which they are based.
£10m OF HEALTHWATCH CASH 'GOES MISSING
13 February, 2014 - HSJ
Nearly a quarter of the funding for local Healthwatch groups has gone missing, according to research by the national body representing them.
13 February, 2014 - HSJ
Nearly a quarter of the funding for local Healthwatch groups has gone missing, according to research by the national body representing them.
CQC APPOINTS WHISTLEBLOWING ADVISOR
Last week, paediatrician Dr Kim Holt began a new role at CQC as a professional advisor providing advice to CQC on issues relating to whistle blowing.
Dr Holt began her new role by leading a workshop with people who have experience of whistleblowing, who discussed the issues they faced and the barriers that can prevent staff from raising concerns.The feedback will help CQC to develop its new approach to regulating health and adult social care services, which will include assessing how providers listen to and treat whistleblowers. The feedback will also give CQC a better understanding of the experiences of staff who raise concerns and the issues whistleblowers face.
Dr Holt formed the campaign group Patients First following her own whistleblowing experiences. In 2007 Dr Holt raised concerns with management over staffing and record keeping at the clinic which failed to spot the abuse which had been suffered by Baby P.
At the CQC, we have dedicated team that manage calls and correspondence from people who would like to raise concerns about healthcare or adult social care services in England – both from those who work in, and from people who use or whose loved ones use, services. In 2012/13, the team received 8,600 contacts – 600 of these were from the NHS and since last April, the team has received over 7,800 (around 730 were from the NHS).
To find out when and how to raise a concern, read our guide. If you have any questions please contact:
Owen Davies
Public Affairs Officer
Care Quality Commission
Finsbury Tower
103-105 Bunhill Row Telephone: 020 7448 1621
London, EC1Y 8TG Email: [email protected]
Last week, paediatrician Dr Kim Holt began a new role at CQC as a professional advisor providing advice to CQC on issues relating to whistle blowing.
Dr Holt began her new role by leading a workshop with people who have experience of whistleblowing, who discussed the issues they faced and the barriers that can prevent staff from raising concerns.The feedback will help CQC to develop its new approach to regulating health and adult social care services, which will include assessing how providers listen to and treat whistleblowers. The feedback will also give CQC a better understanding of the experiences of staff who raise concerns and the issues whistleblowers face.
Dr Holt formed the campaign group Patients First following her own whistleblowing experiences. In 2007 Dr Holt raised concerns with management over staffing and record keeping at the clinic which failed to spot the abuse which had been suffered by Baby P.
At the CQC, we have dedicated team that manage calls and correspondence from people who would like to raise concerns about healthcare or adult social care services in England – both from those who work in, and from people who use or whose loved ones use, services. In 2012/13, the team received 8,600 contacts – 600 of these were from the NHS and since last April, the team has received over 7,800 (around 730 were from the NHS).
To find out when and how to raise a concern, read our guide. If you have any questions please contact:
Owen Davies
Public Affairs Officer
Care Quality Commission
Finsbury Tower
103-105 Bunhill Row Telephone: 020 7448 1621
London, EC1Y 8TG Email: [email protected]
COMPLAINTS AND RAISING CONCERNS
Inquiry announced 03 February 2014:
Written submissions invited, deadline for submissions is 12 noon on Friday, 07 March 2014
http://www.parliament.uk/business/committees/committees-a-z/commons-select/health-committee/inquiries/parliament-2010/complaints-and-raising-concerns/
The Health Committee has decided to review progress in improving the handling of complaints from patients and the public, and concerns raised by staff. Specifically, the inquiry will consider:
Inquiry announced 03 February 2014:
Written submissions invited, deadline for submissions is 12 noon on Friday, 07 March 2014
http://www.parliament.uk/business/committees/committees-a-z/commons-select/health-committee/inquiries/parliament-2010/complaints-and-raising-concerns/
The Health Committee has decided to review progress in improving the handling of complaints from patients and the public, and concerns raised by staff. Specifically, the inquiry will consider:
- Handling of complaints made by patients and families about care received in the health and care sectors, including both primary and secondary care providers;
- Handling of concerns raised by staff about care given in the health and care sectors;
- The extent to which the findings of recent inquiries have been incorporated into the complaints process;
- Support for patients, the public and staff who wish to make complaints or raise concerns;
- The consequences of complaints for care providers and of raising concerns for the employment prospects of staff;
- Openness about complaints and concerns, and accessibility of information;
- The role of commissioners, system regulators and professional regulators with regard to complaints and concerns;
- The operation of the Public Interest Disclosure Act 1998 in relation to health and social care;
- Future plans for improvements in this area.
CARE AND SUPPORT REFORM: SUPPORTING IMPLEMENTATION
By: Kristian Hibbard - 07 February 2014
Catering for the health and care needs of our growing and aging population is a national priority, explains Kristian Hibberd, Communications Manager, Local Government Association.
Reforming our care and support system is vital for us to be able to meet this challenge. As the Care Bill makes its way through Parliament, the health and care sector is preparing to implement the care and support reforms. The Department of Health has partnered with the Local Government Association (LGA) and the Association of Directors of Adult Social Services (ADASS) to deliver a programme of work to support this.
We have launched a website and monthly bulletin for everyone interested in, or responsible for, implementing the reforms. The site includes:
By: Kristian Hibbard - 07 February 2014
Catering for the health and care needs of our growing and aging population is a national priority, explains Kristian Hibberd, Communications Manager, Local Government Association.
Reforming our care and support system is vital for us to be able to meet this challenge. As the Care Bill makes its way through Parliament, the health and care sector is preparing to implement the care and support reforms. The Department of Health has partnered with the Local Government Association (LGA) and the Association of Directors of Adult Social Services (ADASS) to deliver a programme of work to support this.
We have launched a website and monthly bulletin for everyone interested in, or responsible for, implementing the reforms. The site includes:
- information on the £2.7 million implementation fund to be invested across the nine regions
- a getting started guide for those responsible for implementation
- a set of “must knows” for councillors, chief executives and other senior managers
- a clause-by-clause analysis of the Care Bill
- guidance notes for the necessary IT investment, new technologies and information systems.

QUALITY ACCOUNTS
From: NHS England - Patient and Public Voice
Click on the flyer image for dates and details about Quality Accounts sessions.
From: NHS England - Patient and Public Voice
Click on the flyer image for dates and details about Quality Accounts sessions.
HAPIA'S GUIDE TO CASUALTYWATCH 2014
-----------------------------------------------------------
Appendices:
1. Casualty: Evening Standard
2A. Casualty Watch Form
2B. Guidance Notes for Casualty Watch
3. Example of Data Collection
4A. Casualty Data - Homerton University Hospital
4B. Casualty Data - Homerton University Hospital
5A. 30 Minutes Patient Handover Breaches - London
5B. 60 Minutes Patient Handover Breaches - London
REVALIDATION OF DOCTORS
The Role of Case Manager in Improving the Performance of Doctors
Sharing Information with Patients, Carers and the Public
Draft - 9 pages
This Good Practice Guide has been prepared by the Healthwatch and Public Involvement Association (HAPIA) to support Case Managers in understanding the principles and benefits of sharing information with patients, carers and the public when a doctor is undergoing investigation or remediation.
PPI OPPORTUNITIES:
REHABILITATION IS EVERYONE'S BUSINESS - An opportunity to be involved
NHS England is developing principles and objectives for the delivery of high quality adult rehabilitation services. Examples of rehabilitation services include those received after a stroke or brain injury, following a fall, for cardiac and respiratory disease, as well as end of life care. This work also includes the transition from children and young people’s services into adult rehabilitation services. An important aspect of this work is to ensure that equal consideration is given to both mental and physical health in rehabilitation services.
Rehabilitation is everyone’s business – an opportunity to be involved
For further information, events and opportunities … … Click here
REHABILITATION IS EVERYONE'S BUSINESS - An opportunity to be involved
NHS England is developing principles and objectives for the delivery of high quality adult rehabilitation services. Examples of rehabilitation services include those received after a stroke or brain injury, following a fall, for cardiac and respiratory disease, as well as end of life care. This work also includes the transition from children and young people’s services into adult rehabilitation services. An important aspect of this work is to ensure that equal consideration is given to both mental and physical health in rehabilitation services.
Rehabilitation is everyone’s business – an opportunity to be involved
For further information, events and opportunities … … Click here
|
HOSPITAL INSPECTIONS
Intervening in Response to Reports of Declining Services 17 slides PowerPoint Presentation __________________________________________________________________________________ Malcolm Alexander - 16 January 2014 |
NEW HOSPITAL INSPECTIONS
What to Expect and How to Prepare
By: Westminster Briefing
_____________________________________________________________________________________
98 Pages - 16 January 2014
What to Expect and How to Prepare
By: Westminster Briefing
_____________________________________________________________________________________
98 Pages - 16 January 2014