NEWS - JUNE 2015
HWE ON DATA SHARING
Ten Ways to give Patients Confidence in How Their Data is Shared ... 2 pages
Care.data aims to make better use of patient information to improve care in the future. However, consumers reported to us that they felt unable to make an informed decision about whether to opt out of the programme.
After consulting with stakeholders, the programme is now planning 'pathfinder' projects in four areas of England. The projects will test the clarity of the patient communications materials and the effectiveness of the data extraction process.
Ten Ways to give Patients Confidence in How Their Data is Shared ... 2 pages
Care.data aims to make better use of patient information to improve care in the future. However, consumers reported to us that they felt unable to make an informed decision about whether to opt out of the programme.
After consulting with stakeholders, the programme is now planning 'pathfinder' projects in four areas of England. The projects will test the clarity of the patient communications materials and the effectiveness of the data extraction process.
To: [email protected]
Subject: Response to your Query : - Ref:DE00000941001 - Your recent email to the Department of Health
Dear Mrs Marsden,
Thank you for your email of 15 June about ministerial responsibilities. I have been asked to reply.
Ben Gummer MP, Parliamentary Under Secretary of State for Care Quality, has responsibility for patient experience and quality improvement, including oversight of Healthwatch England.
I hope this reply is helpful.
Yours sincerely,
Ryan Diggory
Ministerial Correspondence and Public Enquiries
Department of Health
Subject: Response to your Query : - Ref:DE00000941001 - Your recent email to the Department of Health
Dear Mrs Marsden,
Thank you for your email of 15 June about ministerial responsibilities. I have been asked to reply.
Ben Gummer MP, Parliamentary Under Secretary of State for Care Quality, has responsibility for patient experience and quality improvement, including oversight of Healthwatch England.
I hope this reply is helpful.
Yours sincerely,
Ryan Diggory
Ministerial Correspondence and Public Enquiries
Department of Health
THIRD OF COUNCILS CUT HEALTHWATCH BUDGETS
18 June, 2015
Healthwatch England has demanded explanations from Councils that have imposed deep funding cuts on its local groups this year.
Almost a third of Councils cut local Healthwatch budgets in 2015-16 by an average of 14 per cent, Local Government Chronicle has learned.
Through interviews with 147 of 148 local Healthwatch branches, 10 councils were identified as having cut local Healthwatch budgets by more than the reduction in their overall grant.
18 June, 2015
Healthwatch England has demanded explanations from Councils that have imposed deep funding cuts on its local groups this year.
Almost a third of Councils cut local Healthwatch budgets in 2015-16 by an average of 14 per cent, Local Government Chronicle has learned.
Through interviews with 147 of 148 local Healthwatch branches, 10 councils were identified as having cut local Healthwatch budgets by more than the reduction in their overall grant.
HEALTHWATCH ENGLAND - COMPLAINTS SYSTEM IN HEALTH AND SOCIAL CARE
HWE - Letter and Action Plan - lays out seven points of action for the Government to reform the health and social care complaints system that will create an effective and compassionate system that both gives patients what they need ... and ensures the NHS and social care services can learn from their mistakes.
HWE - Letter and Action Plan - lays out seven points of action for the Government to reform the health and social care complaints system that will create an effective and compassionate system that both gives patients what they need ... and ensures the NHS and social care services can learn from their mistakes.
MONITOR AND TDA TO JOIN UNDER NEW CHIEF
11 June 2015
Monitor and the NHS Trust Development Authority are to work much more closely together and under a single leader, with a new Chief Executive due to be appointed by the end of the summer.
The two organisations will not formally merge this year, a move some have called for. However, it was due to be announced today that they would be moving to work much more closely together. They will work under a single chief executive, an appointment which will be made by the Department of Health in the near future. David Bennett has announced he will not take on this joint position on a permanent basis and will step down. The Department of Health said it wanted to make a new appointment “by the end of the summer”.
The join between the organisation has been described as “a closer relationship”, but details of what this will mean remain unclear. The DH said in a statement today: “This change will mean that all NHS providers, whether they are foundation trusts or trusts, are under the oversight of one chief executive, overseeing teams working closely together.
11 June 2015
Monitor and the NHS Trust Development Authority are to work much more closely together and under a single leader, with a new Chief Executive due to be appointed by the end of the summer.
- Monitor and TDA to work more closer together under a single leader
- David Bennett to leave Monitor in near future
- New chief exec appointed “by the end of the summer”
- The two organisations will not formally merge
The two organisations will not formally merge this year, a move some have called for. However, it was due to be announced today that they would be moving to work much more closely together. They will work under a single chief executive, an appointment which will be made by the Department of Health in the near future. David Bennett has announced he will not take on this joint position on a permanent basis and will step down. The Department of Health said it wanted to make a new appointment “by the end of the summer”.
The join between the organisation has been described as “a closer relationship”, but details of what this will mean remain unclear. The DH said in a statement today: “This change will mean that all NHS providers, whether they are foundation trusts or trusts, are under the oversight of one chief executive, overseeing teams working closely together.
NHS DETAILS RELEASED AGAINST EXPRESS WISHES OF PATIENTS
GUARDIAN NEWSPAPER Press Association
NHS details released against patients' wishes, admits data body . Health and Social Care Information Centre failed to log requests of up to 700,000 patients not to pass on details and says issue ‘may take some time’ to resolve. The Health and Social Care Information Centre has said technical issues led to the data being shared. ‘Basically it’s a mess,’ said Dr Beth McCarron-Nash of the General Practitioners Committee. The body responsible for releasing NHS patient data to organisations including insurance companies has admitted information about patients has been shared against their wishes, it has emerged.
Requests by up to 700,000 patients for details from their records not to be passed on, registered during preparations for the creation of a giant medical database, have not been met. But the Health and Social Care Information Centre (HSCIC) told MPs that it “does not currently have the resources or processes to handle such a significant level of objection” and it also encountered technical issues over logging the preferences.
Patients registered their objections during the development of the controversial Care data system, but the plans were shelved in March 2014. The admission was made in a letter to the House of Commons Health Select Committee in February from HSCIC Chair, Kingsley Manning, who admitted it “may take some time” to resolve the issue.
Dr Beth McCarron-Nash, who leads on care data for the General Practitioners Committee (GPC), told health sector journal Pulse: “Obviously, if there are technical difficulties that HSCIC are experiencing they must be resolved, and it is their responsibility to make sure patients are protected. But basically it’s a mess.”
Phil Booth, director of data rights advocacy group medConfidential told Pulse: “The material fact is, hundreds of thousands of people, last January, February, March, exercised their right to opt out of having their data passed on by the HSCIC, and that has not been respected.”
GUARDIAN NEWSPAPER Press Association
NHS details released against patients' wishes, admits data body . Health and Social Care Information Centre failed to log requests of up to 700,000 patients not to pass on details and says issue ‘may take some time’ to resolve. The Health and Social Care Information Centre has said technical issues led to the data being shared. ‘Basically it’s a mess,’ said Dr Beth McCarron-Nash of the General Practitioners Committee. The body responsible for releasing NHS patient data to organisations including insurance companies has admitted information about patients has been shared against their wishes, it has emerged.
Requests by up to 700,000 patients for details from their records not to be passed on, registered during preparations for the creation of a giant medical database, have not been met. But the Health and Social Care Information Centre (HSCIC) told MPs that it “does not currently have the resources or processes to handle such a significant level of objection” and it also encountered technical issues over logging the preferences.
Patients registered their objections during the development of the controversial Care data system, but the plans were shelved in March 2014. The admission was made in a letter to the House of Commons Health Select Committee in February from HSCIC Chair, Kingsley Manning, who admitted it “may take some time” to resolve the issue.
Dr Beth McCarron-Nash, who leads on care data for the General Practitioners Committee (GPC), told health sector journal Pulse: “Obviously, if there are technical difficulties that HSCIC are experiencing they must be resolved, and it is their responsibility to make sure patients are protected. But basically it’s a mess.”
Phil Booth, director of data rights advocacy group medConfidential told Pulse: “The material fact is, hundreds of thousands of people, last January, February, March, exercised their right to opt out of having their data passed on by the HSCIC, and that has not been respected.”
THE 'SUCCESS REGIME'
Ben Gummer The Parliamentary Under-Secretary of State for Health
I welcome the success regime, details of which were published by Monitor yesterday. The purpose of the success regime is to improve health and care services for patients in local health and care systems that are struggling with financial or quality problems. It will build on the improvements made through the special measures regime, recognising that some of the underlying reasons may result from intrinsic structural problems in the local health economy. This will, therefore, make sure issues are addressed in the region, not just in one organisation.
The regime is designed to make improvements in some of the most challenged health and care economies. The first sites to enter the regime—North Cumbria, Essex and North East and West Devon—are facing some of the most significant challenges in England. They have been selected based on data such as quality metrics, financial performance and other qualitative information.
Unlike under previous interventions, this success regime will look at the whole health and care economy: providers, such as hospital trusts, service commissioners, clinical commissioning groups and local authorities will be central to the discussions. It will be supported by three national NHS bodies, whereas existing interventions tend to be delivered by individual organisations and to concentrate on one part of a health economy—for example, the commissioning assurance framework led by NHS England that concentrates solely on commissioners, or special measures led by NHS England, the Trust Development Authority or Monitor, which focuses on providers.
Together, Monitor, TDA and NHS England, with local commissioners, patients, their representatives such as Healthwatch England and health and wellbeing boards will aim to address systemic issues. The national bodies will provide support all the way through to implementation, with a focus on supporting and developing local leadership through the process.
http://www.theyworkforyou.com/debates/?id=2015-06-04a.753.0&s=healthwatch#g753.3
I welcome the success regime, details of which were published by Monitor yesterday. The purpose of the success regime is to improve health and care services for patients in local health and care systems that are struggling with financial or quality problems. It will build on the improvements made through the special measures regime, recognising that some of the underlying reasons may result from intrinsic structural problems in the local health economy. This will, therefore, make sure issues are addressed in the region, not just in one organisation.
The regime is designed to make improvements in some of the most challenged health and care economies. The first sites to enter the regime—North Cumbria, Essex and North East and West Devon—are facing some of the most significant challenges in England. They have been selected based on data such as quality metrics, financial performance and other qualitative information.
Unlike under previous interventions, this success regime will look at the whole health and care economy: providers, such as hospital trusts, service commissioners, clinical commissioning groups and local authorities will be central to the discussions. It will be supported by three national NHS bodies, whereas existing interventions tend to be delivered by individual organisations and to concentrate on one part of a health economy—for example, the commissioning assurance framework led by NHS England that concentrates solely on commissioners, or special measures led by NHS England, the Trust Development Authority or Monitor, which focuses on providers.
Together, Monitor, TDA and NHS England, with local commissioners, patients, their representatives such as Healthwatch England and health and wellbeing boards will aim to address systemic issues. The national bodies will provide support all the way through to implementation, with a focus on supporting and developing local leadership through the process.
http://www.theyworkforyou.com/debates/?id=2015-06-04a.753.0&s=healthwatch#g753.3
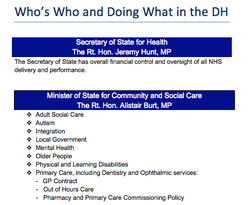
WHO'S WHO and DOING WHAT in the DEPARTMENT OF HEALTH
NEW LEGISLATION
Look out for the Government's Cities and Local Government Devolution Bill, which would give Ministers power to transfer powers from NHS Authorities to new combined city-wide Authorities.
The Legislation is intended to be used for areas like Greater Manchester, where there are proposals for devolved and shared NHS and social care budgets, alongside devolution and sharing of many other functions, but it is as yet unclear how it will be used in practice in relation to the NHS.
Look out for the Government's Cities and Local Government Devolution Bill, which would give Ministers power to transfer powers from NHS Authorities to new combined city-wide Authorities.
The Legislation is intended to be used for areas like Greater Manchester, where there are proposals for devolved and shared NHS and social care budgets, alongside devolution and sharing of many other functions, but it is as yet unclear how it will be used in practice in relation to the NHS.
PUBLIC ENGAGEMENT - CCGs
A Guide to CCGs - Engaging the public in difficult decisions about health service change
NHS Clinical Commissioners - 12 pages - June 2015
NHS Clinical Commissioners (NHSCC) today publishes a guide on how clinical commissioning groups (CCGs) can engage the public in challenging decisions about healthcare transformation.
The Guide offers some top tips on how to get your engagement right:
1: Timing is everything
2: Call the experts
3: Get your messaging right
4: Go wide
5: Listen, be respectful, be honest…and let go
A Guide to CCGs - Engaging the public in difficult decisions about health service change
NHS Clinical Commissioners - 12 pages - June 2015
NHS Clinical Commissioners (NHSCC) today publishes a guide on how clinical commissioning groups (CCGs) can engage the public in challenging decisions about healthcare transformation.
The Guide offers some top tips on how to get your engagement right:
1: Timing is everything
2: Call the experts
3: Get your messaging right
4: Go wide
5: Listen, be respectful, be honest…and let go
Chair of the Lay Member Network, Susanne Hasselmann says:
“The need to engage the public in these changes is vital, but it is not always an easy proposition. Redesigns of health services can illicit [ ??] strong feelings in local communities. CCGs are still learning what works and what doesn’t, and our knowledge about good public engagement is growing. What this guide does is share the expertise and experience of those who have successfully engaged their local communities in change.
“Public engagement is not a process which can be rushed, and CCGs need to work with other local partners, like Healthwatch, to make sure they consult a wide range of people in a wide range of settings. During Healthier Together, for instance, they spread information on the programme through hiring a market stall and partnering with a local radio station at community events.”
Susan Robinson, Head of Development at Healthwatch England, said “It’s encouraging to see this Guide from the NHSCC on engaging the public in discussions about health service change.
“Involving the public in changes to health services from the start of the process is key to getting the best results; the experiences and needs of patients must be listened to and considered when making such important and challenging decisions. Local Healthwatch are a key local partner for all CCGs that want to make this happen, so we would encourage all CCGs to work in partnership with their local Healthwatch when engaging the public on key decisions about health service change.”
Susanne Hasselmann concludes: “An increasing number of Commissioners will be faced with difficult decisions about local services, and with public concern about changes the advice in this guide can therefore only become more important as time goes on. We hope this guide helps our members and others to get those conversations right with the public.”
“The need to engage the public in these changes is vital, but it is not always an easy proposition. Redesigns of health services can illicit [ ??] strong feelings in local communities. CCGs are still learning what works and what doesn’t, and our knowledge about good public engagement is growing. What this guide does is share the expertise and experience of those who have successfully engaged their local communities in change.
“Public engagement is not a process which can be rushed, and CCGs need to work with other local partners, like Healthwatch, to make sure they consult a wide range of people in a wide range of settings. During Healthier Together, for instance, they spread information on the programme through hiring a market stall and partnering with a local radio station at community events.”
Susan Robinson, Head of Development at Healthwatch England, said “It’s encouraging to see this Guide from the NHSCC on engaging the public in discussions about health service change.
“Involving the public in changes to health services from the start of the process is key to getting the best results; the experiences and needs of patients must be listened to and considered when making such important and challenging decisions. Local Healthwatch are a key local partner for all CCGs that want to make this happen, so we would encourage all CCGs to work in partnership with their local Healthwatch when engaging the public on key decisions about health service change.”
Susanne Hasselmann concludes: “An increasing number of Commissioners will be faced with difficult decisions about local services, and with public concern about changes the advice in this guide can therefore only become more important as time goes on. We hope this guide helps our members and others to get those conversations right with the public.”