NEWS - JULY 2014
GUIDANCE ON PUBLISHING NEW CONTRACT OPPORTUNITIES FOR NHS HEALTH CARE SERVICES
This document we focuses on providing guidance for commissioners on the National Health Service (Procurement, Patient Choice and Competition) (No. 2) Regulations 2013. These regulations are also sometimes referred to as the “section 75 regulations” or “the commissioner regulations”. While the regulations replace the previous administrative rules governing the procurement of NHS-funded services set out by the Department of Health (in Principles and rules for cooperation and competition and Procurement guide for commissioners of NHS-funded services), the substance of the former rules is preserved within them.
https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/283505/SubstantiveGuidanceDec2013_0.pdf
This document we focuses on providing guidance for commissioners on the National Health Service (Procurement, Patient Choice and Competition) (No. 2) Regulations 2013. These regulations are also sometimes referred to as the “section 75 regulations” or “the commissioner regulations”. While the regulations replace the previous administrative rules governing the procurement of NHS-funded services set out by the Department of Health (in Principles and rules for cooperation and competition and Procurement guide for commissioners of NHS-funded services), the substance of the former rules is preserved within them.
https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/283505/SubstantiveGuidanceDec2013_0.pdf
CQC SLOWDOWN - Inspection notice periods could treble
30 July, 2014
Hospitals, GP practices and care homes could see pre-inspection notice periods trebled under a new Care Quality Commission approach. The change would see hospitals receive up to 20 weeks’ warning compared with 6-8 weeks currently, the chief inspector of hospitals Sir Mike Richards said. Sir Mike said the move would allow inspectors to “really do some homework” about trusts, including meetings with their commissioners. It would also enable the CQC to recruit the most appropriate experts to assist its inspection teams.
The change was recommended by an academic evaluation of the CQC’s new regulatory model.
The Care Quality Commission has scaled back its inspection ambitions for the rest of 2014-15 as it seeks to ease pressure on its hard pressed workforce and struggles to recruit enough high calibre staff. The regulator’s planned reduction in workload was revealed by its Chief Executive, David Behan, who also admitted some inspection teams were operating with just half their full complement. He said the CQC’s original plan had been “recalibrated” because “we have not recruited the numbers of staff during the early parts of this year we anticipated”. He insisted recruitment of extra inspectors was taking longer than expected because the CQC had set “high standards” for new recruits. He said: “I think we’ve been right to have high standards about who comes into the organisation… we’ve been clear that I’m not going to drop the standards on who comes to work in the CQC.”
30 July, 2014
Hospitals, GP practices and care homes could see pre-inspection notice periods trebled under a new Care Quality Commission approach. The change would see hospitals receive up to 20 weeks’ warning compared with 6-8 weeks currently, the chief inspector of hospitals Sir Mike Richards said. Sir Mike said the move would allow inspectors to “really do some homework” about trusts, including meetings with their commissioners. It would also enable the CQC to recruit the most appropriate experts to assist its inspection teams.
The change was recommended by an academic evaluation of the CQC’s new regulatory model.
The Care Quality Commission has scaled back its inspection ambitions for the rest of 2014-15 as it seeks to ease pressure on its hard pressed workforce and struggles to recruit enough high calibre staff. The regulator’s planned reduction in workload was revealed by its Chief Executive, David Behan, who also admitted some inspection teams were operating with just half their full complement. He said the CQC’s original plan had been “recalibrated” because “we have not recruited the numbers of staff during the early parts of this year we anticipated”. He insisted recruitment of extra inspectors was taking longer than expected because the CQC had set “high standards” for new recruits. He said: “I think we’ve been right to have high standards about who comes into the organisation… we’ve been clear that I’m not going to drop the standards on who comes to work in the CQC.”
DECLINE IN FUNDING FOR GPs - NHS ENGLAND BOARD PAPERS
The Government’s spending on GP services appeared to decline by 2.3% last year compared to the previous year, according to figures released by the Department of Health.
According to DH annual accounts, published yesterday, total spend on GMS, PMS and non-GMS GP services was £7.55bn in 2013/14, compared with £7.73bn in 2012/13. This comes despite overall DH spend rising by 2.6%, including increased spending on bailing out hospital trusts and buying healthcare services from non-NHS providers, which topped £10bn for the first time. It comes after NHS England board papers published in May revealed that it had made savings on primary care costs despite recording a huge overspend overall, but NHS England claimed it was not possible to directly compare their accounts to legacy PCT accounts.
The Government’s spending on GP services appeared to decline by 2.3% last year compared to the previous year, according to figures released by the Department of Health.
According to DH annual accounts, published yesterday, total spend on GMS, PMS and non-GMS GP services was £7.55bn in 2013/14, compared with £7.73bn in 2012/13. This comes despite overall DH spend rising by 2.6%, including increased spending on bailing out hospital trusts and buying healthcare services from non-NHS providers, which topped £10bn for the first time. It comes after NHS England board papers published in May revealed that it had made savings on primary care costs despite recording a huge overspend overall, but NHS England claimed it was not possible to directly compare their accounts to legacy PCT accounts.
CUT HOSPITAL DOCTOR TRAINING TO EXPAND GP RECRUITMENT
63 pages
Hospital specialist training places should be radically cut back to make way for a rapid expansion in GP recruits, recommends a major report into how to boost GP numbers commissioned by ministers.
The ‘GP taskforce’ report recommends that GP training numbers are increased alongside a ‘concomitant reduction in hospital specialty places’ and suggests 2,025 hospital training places could be decommissioned to achieve this aim.
63 pages
Hospital specialist training places should be radically cut back to make way for a rapid expansion in GP recruits, recommends a major report into how to boost GP numbers commissioned by ministers.
The ‘GP taskforce’ report recommends that GP training numbers are increased alongside a ‘concomitant reduction in hospital specialty places’ and suggests 2,025 hospital training places could be decommissioned to achieve this aim.
The report commissioned by the Department of Health and written by GP education leaders looks at ways of boosting the numbers of GP postgraduate training places to 50% of all places by 2015 - since postponed to 2016 - or 3,250 GPs entering training every year. It says there is a need to ‘redress the imbalance’ between hospital doctors and GPs and calls for a review of current targets to see if they training would be enough to meet workforce needs. It also questioned whether Health Education England would be able to meet the current target of 3,250 GPs, mandated by the DH.
Other radical recommendations include introducing a ‘federated model’ of GP training, which will enable non-training practices to play a role, an incentive scheme for trainees to go to deprived areas and a national funding scheme to help GPs return to General Practice.
Other radical recommendations include introducing a ‘federated model’ of GP training, which will enable non-training practices to play a role, an incentive scheme for trainees to go to deprived areas and a national funding scheme to help GPs return to General Practice.

COUNCILS URGED TO TOUGHEN HEALTH SCRUTINY
07 July, 2014 - 24 pages
Local Authorities have been urged to step up their scrutiny of NHS providers, as a survey revealed funding for such checks has dwindled. The call for strengthening council probes of healthcare services came in new guidance by the Department of Health. [see circulation of 1/7/14]
This suggested local health scrutiny committees should actively seek out information about service quality. “Health scrutiny has a legitimate role in proactively seeking information about the performance of local health services and institutions in challenging the information provided to it… and in testing this information by drawing on different sources of intelligence,” it stated. The guidance added that health scrutiny must “consider ways of independently verifying information provided by relevant NHS bodies and relevant health service providers. For example, by seeking the views of local Healthwatch”.
The “primary aim” of health scrutiny should be to strengthen the voice of local people and ensure their experiences of healthcare are part of the process, it added. Council checks were described as an “unreliable detector of concerns” in health services by Sir Robert Francis QC, following the public inquiry he led into care failings at Stafford Hospital. He described Staffordshire County Council’s scrutiny committee as being “wholly ineffective”, and argued “scrutiny ought to involve more than the passive and unchallenging receipt of reports”.
The DH’s call to action came as an annual survey by the Centre for Public Scrutiny last week pointed to falling resources for council scrutiny committees, including a drop in the number of officers and budgets set aside. It found dedicated scrutiny budgets had declined from £4,015 on average in 2013-14 to £3,447 in 2014-15 – the lowest level since 2004.
Katie Hall, chair of the Local Government Association’s Community Wellbeing Board, said: “Councils recognise that health scrutiny is vital in providing local accountability and challenge to the health system. “The LGA and Centre for Public Scrutiny continue to work together to support councillors to ensure their health scrutiny function works closely with patient and public engagement organisations, and health and wellbeing boards to drive continuous improvement of local health services.”
07 July, 2014 - 24 pages
Local Authorities have been urged to step up their scrutiny of NHS providers, as a survey revealed funding for such checks has dwindled. The call for strengthening council probes of healthcare services came in new guidance by the Department of Health. [see circulation of 1/7/14]
This suggested local health scrutiny committees should actively seek out information about service quality. “Health scrutiny has a legitimate role in proactively seeking information about the performance of local health services and institutions in challenging the information provided to it… and in testing this information by drawing on different sources of intelligence,” it stated. The guidance added that health scrutiny must “consider ways of independently verifying information provided by relevant NHS bodies and relevant health service providers. For example, by seeking the views of local Healthwatch”.
The “primary aim” of health scrutiny should be to strengthen the voice of local people and ensure their experiences of healthcare are part of the process, it added. Council checks were described as an “unreliable detector of concerns” in health services by Sir Robert Francis QC, following the public inquiry he led into care failings at Stafford Hospital. He described Staffordshire County Council’s scrutiny committee as being “wholly ineffective”, and argued “scrutiny ought to involve more than the passive and unchallenging receipt of reports”.
The DH’s call to action came as an annual survey by the Centre for Public Scrutiny last week pointed to falling resources for council scrutiny committees, including a drop in the number of officers and budgets set aside. It found dedicated scrutiny budgets had declined from £4,015 on average in 2013-14 to £3,447 in 2014-15 – the lowest level since 2004.
Katie Hall, chair of the Local Government Association’s Community Wellbeing Board, said: “Councils recognise that health scrutiny is vital in providing local accountability and challenge to the health system. “The LGA and Centre for Public Scrutiny continue to work together to support councillors to ensure their health scrutiny function works closely with patient and public engagement organisations, and health and wellbeing boards to drive continuous improvement of local health services.”
INFORMATION FOR HEALTHWATCH 67
23 July 2014
Information for Healthwatch aims to pick up DH, CQC, LGA, NHSE, HWE, Monitor and other reports that Local Healthwatch will need to know about and to pass on other information I glean from other sources, including the King's Fund Health Policy and Management Alerts, Social Care Institute for Excellence, National Voices and HAPIA. It can't be comprehensive, so if you know of anything I should include please let me know, E&OE!
To view the topics and the links, click here ...
* Older people and the quality of life * NHSE Bulletin for CCGs
* Mortality measurement: the case in favour * Consultation on the 2015-2016 Tariff and payments system
* Monitor FT Bulletin * Friends and Family Test Review
* Understanding the rise in Fitness to Practice complaints from members of the public
* Congenital Heart Disease Review
23 July 2014
Information for Healthwatch aims to pick up DH, CQC, LGA, NHSE, HWE, Monitor and other reports that Local Healthwatch will need to know about and to pass on other information I glean from other sources, including the King's Fund Health Policy and Management Alerts, Social Care Institute for Excellence, National Voices and HAPIA. It can't be comprehensive, so if you know of anything I should include please let me know, E&OE!
To view the topics and the links, click here ...
* Older people and the quality of life * NHSE Bulletin for CCGs
* Mortality measurement: the case in favour * Consultation on the 2015-2016 Tariff and payments system
* Monitor FT Bulletin * Friends and Family Test Review
* Understanding the rise in Fitness to Practice complaints from members of the public
* Congenital Heart Disease Review
HEATHWATCH WARNS OF THE RISE OF 'SUPER CCGs'
HSJ - 22 July 2014
The Health Secretary has been urged to rethink legal reforms that would ease the creation of allegedly unaccountable “super clinical commissioning groups”.
In a letter dispatched to Jeremy Hunt last week, Healthwatch England Chair, Anna Bradley, said local Healthwatch organisations had become concerned about CCGs “clubbing together” in closed groups to discuss reshaping health services across wide areas. Such set ups circumvented local scrutiny and accountability measures, undermining Healthwatch’s statutory role, the letter stated.
“Local Healthwatch have escalated concerns to us about the transparency and accountability of decision making and the effect it is having on their ability to carry out their statutory functions,” it added.
The letter urged Mr Hunt to amend a legal instrument, currently passing through Parliament, that will make it easier for CCGs to form joint committees and delegate a single CCG to make decisions on behalf of all the member groups.
Ms Bradley said the Health Secretary needed to strengthen the “accountability measures” of the Legislative Reform (Clinical Commissioning Groups) Order 2014, by introducing a legal amendment at the “next legislative opportunity”.
The order cannot be redrafted at this stage of its passage through Parliament.
Under amendments proposed in the letter, Healthwatch representatives would be given a mandatory non-voting seat on any committees formed by CCGs. Currently, CCGs are not legally required to give local Healthwatch representatives a seat on either their individual committees or on any they establish.
Ms Bradley has also called for a duty to be placed on all lead or co-ordinating commissioners, to “act within existing local accountability mechanisms” and “have due regard to existing local agreed priorities and plans”. She has also advised the Department of Health to jointly issue statutory guidance that places a “requirement on CCGs to enhance their public engagement and involvement when working in collaboration or under joint commissioning arrangements”.
Marc Bush, Director of Policy and Intelligence for Healthwatch, told HSJ that he has noticed a “greater appetite” among CCGS for “regional based commissioning”.
“What we’re finding is that middle level is increasingly - because of the financial restraints - the level that people are having to make or talk about difficult decisions,” he said. He added that effective accountability structures “only exist at a national or local level”.
“You [will] end with decisions being taken by people who are not connected with the areas that are being affected,” Mr Bush said. “The decisions they’re making are at such a huge scale and involve such important questions about reconfiguration that [commissioners] … can’t afford not to take the public with them on that journey. “Poor engagement in the decision-making process will end up in them having to face long protracted campaigns from local residents not wanting [services] to close down as a result of any decision they weren’t involved in.”
Steve Kell, Co-chair of NHS Clinical Commissioners, said: “We would reject the need for any further statutory or mandatory top-down requirements or reorganisation of CCGs. Having a joint committee doesn’t take away any of the statutory responsibilities of… patient and public engagement. CCGs still need to ensure they have strong transparent and accountable patient and population engagement in their plans, through Healthwatch and local CCG mechanisms.”
HSJ - 22 July 2014
The Health Secretary has been urged to rethink legal reforms that would ease the creation of allegedly unaccountable “super clinical commissioning groups”.
In a letter dispatched to Jeremy Hunt last week, Healthwatch England Chair, Anna Bradley, said local Healthwatch organisations had become concerned about CCGs “clubbing together” in closed groups to discuss reshaping health services across wide areas. Such set ups circumvented local scrutiny and accountability measures, undermining Healthwatch’s statutory role, the letter stated.
“Local Healthwatch have escalated concerns to us about the transparency and accountability of decision making and the effect it is having on their ability to carry out their statutory functions,” it added.
The letter urged Mr Hunt to amend a legal instrument, currently passing through Parliament, that will make it easier for CCGs to form joint committees and delegate a single CCG to make decisions on behalf of all the member groups.
Ms Bradley said the Health Secretary needed to strengthen the “accountability measures” of the Legislative Reform (Clinical Commissioning Groups) Order 2014, by introducing a legal amendment at the “next legislative opportunity”.
The order cannot be redrafted at this stage of its passage through Parliament.
Under amendments proposed in the letter, Healthwatch representatives would be given a mandatory non-voting seat on any committees formed by CCGs. Currently, CCGs are not legally required to give local Healthwatch representatives a seat on either their individual committees or on any they establish.
Ms Bradley has also called for a duty to be placed on all lead or co-ordinating commissioners, to “act within existing local accountability mechanisms” and “have due regard to existing local agreed priorities and plans”. She has also advised the Department of Health to jointly issue statutory guidance that places a “requirement on CCGs to enhance their public engagement and involvement when working in collaboration or under joint commissioning arrangements”.
Marc Bush, Director of Policy and Intelligence for Healthwatch, told HSJ that he has noticed a “greater appetite” among CCGS for “regional based commissioning”.
“What we’re finding is that middle level is increasingly - because of the financial restraints - the level that people are having to make or talk about difficult decisions,” he said. He added that effective accountability structures “only exist at a national or local level”.
“You [will] end with decisions being taken by people who are not connected with the areas that are being affected,” Mr Bush said. “The decisions they’re making are at such a huge scale and involve such important questions about reconfiguration that [commissioners] … can’t afford not to take the public with them on that journey. “Poor engagement in the decision-making process will end up in them having to face long protracted campaigns from local residents not wanting [services] to close down as a result of any decision they weren’t involved in.”
Steve Kell, Co-chair of NHS Clinical Commissioners, said: “We would reject the need for any further statutory or mandatory top-down requirements or reorganisation of CCGs. Having a joint committee doesn’t take away any of the statutory responsibilities of… patient and public engagement. CCGs still need to ensure they have strong transparent and accountable patient and population engagement in their plans, through Healthwatch and local CCG mechanisms.”
HEALTHWATCH NEEDS TO PUNCH ITS WEIGHT
HSJ - 22 July 2014
As we report this week, Healthwatch England have written to Jeremy Hunt complaining that clinical commissioning groups are excluding patients and service users from consultations on service reconfigurations. It is good to see Healthwatch beginning to flex its muscles.
One of the reasons that CCGs are likely to feel comfortable in not involving the watchdog’s local organisations, is that many of them have yet to establish sufficient credibility with their health economy partners. Some of the blame for this must also lie with the national body, which has punched below its weight.
Chief Executive Anna Bradley’s direct challenge to commissioners and impending government legislation ,appears to mark a more robust approach. However, perhaps the most significant aspect of the Healthwatch challenge is that it springs from perfectly understandable behaviour by CCGs - the desire to make decisions across wider areas than that covered by a single group.
‘Perhaps the most significant aspect of the Healthwatch challenge is that it springs from perfectly understandable behaviour by CCGs’
This, of course, speaks directly to the key conundrum in service reconfiguration - that the best results are often achieved at a scale which makes local involvement the most problematic.
The noise around public involvement in health service changes will grow as the election nears. Labour, for example, is exploring the creation of a new agency for running public consultations.
All options, however, seem doomed to fail unless the government and the NHS are successful in reframing the conversation as one which, first, sets out clearly the likely outcomes if change does not occur and, second, how a national endeavour like the NHS will inevitably mean trade-offs between regions, patient groups and organisations if it is to remain sustainable.
HSJ - 22 July 2014
As we report this week, Healthwatch England have written to Jeremy Hunt complaining that clinical commissioning groups are excluding patients and service users from consultations on service reconfigurations. It is good to see Healthwatch beginning to flex its muscles.
One of the reasons that CCGs are likely to feel comfortable in not involving the watchdog’s local organisations, is that many of them have yet to establish sufficient credibility with their health economy partners. Some of the blame for this must also lie with the national body, which has punched below its weight.
Chief Executive Anna Bradley’s direct challenge to commissioners and impending government legislation ,appears to mark a more robust approach. However, perhaps the most significant aspect of the Healthwatch challenge is that it springs from perfectly understandable behaviour by CCGs - the desire to make decisions across wider areas than that covered by a single group.
‘Perhaps the most significant aspect of the Healthwatch challenge is that it springs from perfectly understandable behaviour by CCGs’
This, of course, speaks directly to the key conundrum in service reconfiguration - that the best results are often achieved at a scale which makes local involvement the most problematic.
The noise around public involvement in health service changes will grow as the election nears. Labour, for example, is exploring the creation of a new agency for running public consultations.
All options, however, seem doomed to fail unless the government and the NHS are successful in reframing the conversation as one which, first, sets out clearly the likely outcomes if change does not occur and, second, how a national endeavour like the NHS will inevitably mean trade-offs between regions, patient groups and organisations if it is to remain sustainable.

FRIENDS AND FAMILY TEST ROLLED OUT TO GP PRACTICES
7 Pages
From 1 December 2014, it is a contractual requirement that all GP practices implement the NHS Friends and Family Test (FFT).
This summary of the guidance is intended to give an overview of the guidance published jointly by NHS Employers, NHS England and the BMA General Practitioners Committee. It does not replace it and people implementing the FFT should read the full guidance.
The full guidance can be found here: www.nhsemployers.org/FFT
NHS England has also published guidance for other parts of the NHS, which includes additional advice, and support to help with implementation, including advice on how to make FFT inclusive. This can be found here: www.england.nhs.uk/wp- content/uploads/2014/07/fft-imp-guid-14.pdf
7 Pages
From 1 December 2014, it is a contractual requirement that all GP practices implement the NHS Friends and Family Test (FFT).
This summary of the guidance is intended to give an overview of the guidance published jointly by NHS Employers, NHS England and the BMA General Practitioners Committee. It does not replace it and people implementing the FFT should read the full guidance.
The full guidance can be found here: www.nhsemployers.org/FFT
NHS England has also published guidance for other parts of the NHS, which includes additional advice, and support to help with implementation, including advice on how to make FFT inclusive. This can be found here: www.england.nhs.uk/wp- content/uploads/2014/07/fft-imp-guid-14.pdf
DEPARTMENT OF HEALTH NON-EXECUTIVE APPOINTMENTS
From: Department of Health - Updated 07 July 2014
Patient and Public Voice Advisory Group (PPVAG), Mr Jason Stamp, has been appointed Chair for 3 years from
12 May 2014. He will receive £150 per day for a minimum time commitment of 24 days per year.
The following have been appointed as members from 12 May 2014:
Members who are not supported by their own organisations to attend will receive a fee of £150 per meeting, covering a half day meeting and a half day preparation, for a time commitment of 10-12 meetings per year, with potential to attend additional meetings periodically, which relate to the work of the assurance group.
https://www.gov.uk/government/publications/dh-non-executive-appointments
From: Department of Health - Updated 07 July 2014
Patient and Public Voice Advisory Group (PPVAG), Mr Jason Stamp, has been appointed Chair for 3 years from
12 May 2014. He will receive £150 per day for a minimum time commitment of 24 days per year.
The following have been appointed as members from 12 May 2014:
- Ms Suzanna Hopwood Mr John James Mr Terence Lewis Mr Steve McNeice
- Ms Neeta Metha JP Ms Sue Millman Mrs Farrah Pradhan Mr Keith Wyncoll
Members who are not supported by their own organisations to attend will receive a fee of £150 per meeting, covering a half day meeting and a half day preparation, for a time commitment of 10-12 meetings per year, with potential to attend additional meetings periodically, which relate to the work of the assurance group.
https://www.gov.uk/government/publications/dh-non-executive-appointments
|
TODAY'S NHS - WHAT'S WHAT
NHS England has produced a new guide to Understanding the New NHS which outlines the organisations and systems that define, sustain and regulate the NHS. This Guide replaces a previous Guide commissioned by Sir Bruce Keogh for junior doctors, and incorporates changes to the structure and function of the NHS. The Guide provides an understandable and informative Guide for everyone working and training within the NHS. |
PRIMARY CARE SUPPORT SERVICES OUT FOR PUBLIC PROCUREMENT
NHS England has today announced the decision to launch an open public procurement process for primary care support services (PCS). To ensure the best deal for primary care and the taxpayer, NHS England has decided an open procurement process is the preferred option. Karen Wheeler said: “NHS England is committed to cutting administrative costs for all services, and these changes will benefit patients and the taxpayer by freeing up more money for care.
Further details of the procurement process are in development. In the meantime the services will continue to be run by NHS England.
NHS England has today announced the decision to launch an open public procurement process for primary care support services (PCS). To ensure the best deal for primary care and the taxpayer, NHS England has decided an open procurement process is the preferred option. Karen Wheeler said: “NHS England is committed to cutting administrative costs for all services, and these changes will benefit patients and the taxpayer by freeing up more money for care.
Further details of the procurement process are in development. In the meantime the services will continue to be run by NHS England.
PRESCRIPTIONS - RATES AND IMPLICATIONS
The report shows for the first time that 60% of free prescriptions – which account for 90% of the total – are given to patients with an ‘over 60s’ charges exemption, and that these account for 51% of the total costs of the drugs.
- The numbers of items prescribed by GPs and other community providers in 2013 increased by more than 30 million, a 3% rise from 2012, figures released by the NHS information centre reveal.
- The ‘Prescriptions Dispensed in the Community 2003-2013’ report by the Health and Social Care Information Centre also shows prescribing jumped 59% since 2003, but that the costs of the drugs only rose 15%.
The report shows for the first time that 60% of free prescriptions – which account for 90% of the total – are given to patients with an ‘over 60s’ charges exemption, and that these account for 51% of the total costs of the drugs.
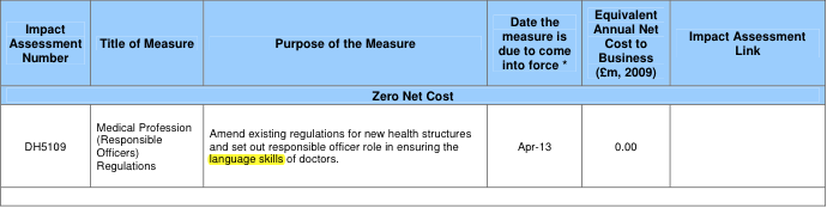
LANGUAGE SKILLS FOR DOCTORS
Information for Healthwatch aims to pick up DH, CQC, LGA, NHSE, HWE Monitor and other reports that Local Healthwatch will need to know about and to pass on other information I glean from other sources, including the King's Fund Health Policy and Management Alerts and HAPIA (NALM). It can't be comprehensive, so if you know of anything I should include please let me know. geoffrey.smith@btinternet.com
Topics: Click here to download the Report and links ...
Topics: Click here to download the Report and links ...
- NHSE Bulletin for CCGs - Issue 62
- Commissioning of public health services for children
- Access all ages 2: exploring variations in access to surgery among older people
- Personalised care
- The Dalton Review - an opportunity for Healthwatch
- Advising residents on health and social care complaints: a councillors' guide
- The CentreForum atlas of variation
- Congenital Heart Disease Review
Wednesday, 23 July - Healthwatch England Public Committee Meeting
Location: Jurys Inn Nottingham City Centre, Station St, Nottingham NG2 3BJ
Agenda and papers to follow.
- There will be a public lunch before the meeting, so that attendees can meet the Committee informally.
- Lunch will start at 12.00pm and the meeting will begin at 12.45pm.
If you have a question for the committee please email enquiries@healthwatch.co.uk
Wednesday, 22 October - Healthwatch England Public Committee Meeting
Our Committee Meeting in October will take place in London ... venue to be confirmed.
Location: Jurys Inn Nottingham City Centre, Station St, Nottingham NG2 3BJ
Agenda and papers to follow.
- There will be a public lunch before the meeting, so that attendees can meet the Committee informally.
- Lunch will start at 12.00pm and the meeting will begin at 12.45pm.
If you have a question for the committee please email enquiries@healthwatch.co.uk
Wednesday, 22 October - Healthwatch England Public Committee Meeting
Our Committee Meeting in October will take place in London ... venue to be confirmed.
Information for Healthwatch aims to pick up DH, CQC, LGA, NHSE, HWE Monitor and other reports that Local Healthwatch will need to know about and to pass on other information I glean from other sources, including the King's Fund Health Policy and Management Alerts and HAPIA (NALM). It can't be comprehensive, so if you know of anything I should include please let me know, E&OE!
- Commissioning for outcomes : a narrative from and for clinical commissioners
- One chance to get it right: improving people's experience of care in the last few days and hours of life
- Understanding the new NHS: a guide for everyone working and training within the NHS
- Commissioning home care for older people
- Health scrutiny by local authorities and their partners
- Nuffield Trust report: meeting or fuelling patient demand?
- Future organisation models for the NHS: perspectives for the Dalton Review
- National conversation on health inequalities
DATA DELETION CANNOT BE ENFORCED
The Health and Social Care Information Centre has admitted it has no power to force private companies holding potentially sensitive patient data obtained from its predecessor body to comply with its requests to delete the information. The Centre announced last month it had written to three re-insurance companies asking them to delete patient data they had obtained legally from the NHS Information Centre.
New regulations are to be introduced under the Care Act this autumn restricting the flow of potentially identifiable data solely to purposes of benefit to the health and social care systems. But HSCIC non-executive director Sir Nick Partridge yesterday told the Commons health committee that one of the companies, SCOR, had refused to agree to delete or stop using the patient data.
The Centre’s Chair, Kingley Manning, added: “I am advised that we do not have powers to ask them to delete the data under the current sharing data agreement.”
The data sharing agreements had originally been drawn up by the HSCIC’s predecessor, the NHS Information Centre.
The Health and Social Care Information Centre has admitted it has no power to force private companies holding potentially sensitive patient data obtained from its predecessor body to comply with its requests to delete the information. The Centre announced last month it had written to three re-insurance companies asking them to delete patient data they had obtained legally from the NHS Information Centre.
New regulations are to be introduced under the Care Act this autumn restricting the flow of potentially identifiable data solely to purposes of benefit to the health and social care systems. But HSCIC non-executive director Sir Nick Partridge yesterday told the Commons health committee that one of the companies, SCOR, had refused to agree to delete or stop using the patient data.
The Centre’s Chair, Kingley Manning, added: “I am advised that we do not have powers to ask them to delete the data under the current sharing data agreement.”
The data sharing agreements had originally been drawn up by the HSCIC’s predecessor, the NHS Information Centre.
GENDER REASSIGNMENT SERVICE AT CHARING CROSS HOSPITAL
Letter from: Dr. Tracey Batten, Chief Executive - Imperial College Healthcare - 24 June 2014
Email from: Malcolm Alexander, Chair, HAPIA - 23 June 2014
Letter from: Dr. Tracey Batten, Chief Executive - Imperial College Healthcare - 24 June 2014
Email from: Malcolm Alexander, Chair, HAPIA - 23 June 2014
EXTRACTS FROM BOARD MEETING WITH NHS ENGLAND
The Chairman commented that, as a national organisation, the National Directors need to engage with staff, patients and providers across the country, not just from centrally located offices.
The Chairman commented that, as a national organisation, the National Directors need to engage with staff, patients and providers across the country, not just from centrally located offices.
- Mr Devane, Chair of the independent care.data advisory group, confirmed that stakeholders supported the implementation with appropriate safeguards in place. The advisory group was engaging with patients and patient organisations regarding the scope of the programme now and into the future. There would be a series of workshops held around the country between now and the autumn.
- In response to a question from the Chairman, it was confirmed that currently GPs may still charge for patients receiving paper copies of their health records.
- Overall, CCGs had 393 contracts with providers, and area teams had 291 contracts for specialised commissioning. The Board noted the progress made against the contract tracker, recognising that a small number were anticipated to go to arbitration.
- Primary care support services - 20% were already outsourced, the remaining 80% having been transferred to NHS England from PCTs.
- CCGs’ contracting position with providers, as of 18 June 2014, 274 out of a total of 388 contracts nationally have been signed. 114 contracts are outstanding, with 88 where the contract activity and financial values have been agreed, and 26 where the contract activity and financial values have not been agreed
- Funding previously described as ‘winter monies’ is this year being directed towards a new approach to year-round system resilience planning. A portion of the money will be retained centrally e.g. for ambulance services, NHS 111 and additional specialised beds, with remaining funds allocated to CCGs in proportion to the size of their population for oversight through SRGs.
- Further money has been released to secure additional elective activity to improve performance on 18 week referral to treatment standards, clear backlog and reduce the number of patients waiting for longer than they should. This money has been allocated to NHS England.
- Many of the fundamental issues remain – growth in activity, new technologies and drugs – and our ability to manage these services, both within 2014-15 and beyond, remains a huge challenge.