NEWS - NOVEMBER 2014
FOUNDATION TRUST OR AN INDEPENDENT MUTUALLY OWNED COMPANY?
NHS Trusts could, in future, choose between becoming a Foundation Trust or an independent mutually owned company as the provider sector becomes increasingly ‘fluid and uncertain’.
The possibility of the mutuals option comes as the Department of Health announced the nine “pathfinder” Trusts which are exploring models of staff ownership under its on going mutuals programme. The Trusts are all investigating whether becoming a mutual would benefit them, through boosting staff engagement.
The nine Pathfinder Trusts are:
NHS Trusts could, in future, choose between becoming a Foundation Trust or an independent mutually owned company as the provider sector becomes increasingly ‘fluid and uncertain’.
The possibility of the mutuals option comes as the Department of Health announced the nine “pathfinder” Trusts which are exploring models of staff ownership under its on going mutuals programme. The Trusts are all investigating whether becoming a mutual would benefit them, through boosting staff engagement.
The nine Pathfinder Trusts are:
- Cheshire and Wirral Partnership Foundation Trust
- Liverpool Heart and Chest Hospital Foundation Trust
- Moorfields Eye Hospital Foundation Trust
- Norfolk and Norwich University Hospitals Foundation Trust
- Norfolk and Suffolk Foundation Trust
- Oxleas Foundation Trust
- Surrey and Sussex Healthcare Trust
- Tameside Hospital Foundation Trust
- University Hospitals of Leicester Trust
|
COMPLAINTS REPORT
Parliamentary and Health Service Ombudsman We have today published a report detailing how many complaints we have investigated for each of England’s 156 hospital trusts and the decisions we made on these complaints, in 2013-14 and the first half of this financial year. The top three reasons for hospital complaints investigated by the Ombudsman Service were poor communication, errors in diagnosis - including delays in diagnosis, misdiagnosis and failure to diagnose - and poor treatment. Other reasons for complaints in this period were staff attitude, no apology when things go wrong and unnecessary delay in treatment. |
|
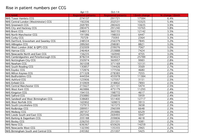
MORE PATIENTS PER GP?
Some GP Practices are facing a huge rise in patient registrations, with average list sizes increasing by up to 500 patients in some CCG areas in the past 18 months. Check out on the attached list what is happening in your CCG area. |
|
CQC CANNOT KEEP UP INSPECTIONS
CQC Chief Executive, David Behan, described recruitment at the regulator as a “key risk”, predicting it would not have a full complement of Inspectors until the end of next year. |
NHS ENGLAND OUTSIDE THE LAW, FLOUTING KEY SECTIONS OF THE NHS ACT
NHS England primary care decisions 'unlawful', High Court rules
24 November
NHS England is acting unlawfully by failing to properly involve and inform patients about its primary care commissioning decisions, a High Court judge has said.
In a ruling with wide ranging implications for the commissioning body, Justice Popplewell last week found NHS England had and continued to flout key sections of the NHS Act. These require commissioners to ensure individual patients are consulted or informed about the “development and consideration” of decisions about or changes to primary care where they affect health services they might use.
The lawyers who brought the case claim NHS England could now face legal challenges over its historic decisions about primary commissioning. According to court papers, Justice Popplewell declared that NHS England “has acted unlawfully by reason of its failure to make arrangements for the involvement of patients in primary care commissioning decisions as required by the National Health Service Act 2006”.
The case was bought by lawyers from Leigh Day on behalf of Danny Currie, a patient registered at the Jubilee Street Practice in Tower Hamlets, which was threatened with closure after NHS England scrapped the minimum Practice Income Guarantee. Although the commissioning body later agreed a two year funding agreement for the Practice, lawyers for Leigh Day argued that patients such as Mr Currie should be involved in any decision that affected services they used.
Richard Stein, a partner at Leigh Day, said that the judge’s declaration “confirms that NHS England will be taking decisions about dealing with GP practices and the sector every day which are in fact unlawful until they put proper arrangements in place as they are required by law”.
“It is shocking that the body responsible nationally for producing guidance for other bodies to carry out these obligations haven’t done so themselves.”
Mr Stein said the declaration could mean that patients would have to be involved in discussions on changes to the GP contract, which are currently being held between NHS England and the British Medical Association. According to the court papers, NHS England conceded it had acted unlawfully, telling the court it was “taking active steps to bring itself into compliance with this duty”.
NHS England has yet to respond.
NHS England primary care decisions 'unlawful', High Court rules
24 November
NHS England is acting unlawfully by failing to properly involve and inform patients about its primary care commissioning decisions, a High Court judge has said.
In a ruling with wide ranging implications for the commissioning body, Justice Popplewell last week found NHS England had and continued to flout key sections of the NHS Act. These require commissioners to ensure individual patients are consulted or informed about the “development and consideration” of decisions about or changes to primary care where they affect health services they might use.
The lawyers who brought the case claim NHS England could now face legal challenges over its historic decisions about primary commissioning. According to court papers, Justice Popplewell declared that NHS England “has acted unlawfully by reason of its failure to make arrangements for the involvement of patients in primary care commissioning decisions as required by the National Health Service Act 2006”.
The case was bought by lawyers from Leigh Day on behalf of Danny Currie, a patient registered at the Jubilee Street Practice in Tower Hamlets, which was threatened with closure after NHS England scrapped the minimum Practice Income Guarantee. Although the commissioning body later agreed a two year funding agreement for the Practice, lawyers for Leigh Day argued that patients such as Mr Currie should be involved in any decision that affected services they used.
Richard Stein, a partner at Leigh Day, said that the judge’s declaration “confirms that NHS England will be taking decisions about dealing with GP practices and the sector every day which are in fact unlawful until they put proper arrangements in place as they are required by law”.
“It is shocking that the body responsible nationally for producing guidance for other bodies to carry out these obligations haven’t done so themselves.”
Mr Stein said the declaration could mean that patients would have to be involved in discussions on changes to the GP contract, which are currently being held between NHS England and the British Medical Association. According to the court papers, NHS England conceded it had acted unlawfully, telling the court it was “taking active steps to bring itself into compliance with this duty”.
NHS England has yet to respond.
PHARMACIST PRESCRIBERS NOT REGULATED THE SAME AS OTHER PRESCRIBERS
Next step for CCGs: co-commissioning pharmacy, dentistry and eye careWhy are pharmacist prescribers not regulated the same as other prescribers?
13 November 2014
There appears to be a gap in the prescribing regulations, writes Dr Tony Steele, medical director of Dr Fox online doctors and pharmacy service. Doctors and all other independent prescriber groups, such as nurse prescribers, work under the auspices of the Care Quality Commission (CQC) - except for pharmacy prescribers.
If a doctor wishes to provide a private diagnostic and prescription service, CQC registration is required. A pharmacist prescriber undertaking similar work is not required to register with the CQC. This may sound like a minor matter, but the CQC has a comprehensive process of registration which looks at all aspects of service provision. Registration usually involves an inspection, interview, a fee and annual reporting, audit and re-inspection.
The General Pharmaceutical Council (GPhC), which oversees pharmacy prescribing, does not have a similar process for registering and monitoring pharmacy prescribing services. Pharmacist prescribers are not revalidated in the same way as doctors.
This anomaly throws up some interesting questions for regulators, particularly in the internet age. Pharmacists are increasingly prescribing online and not always to the same standards. The patients of pharmacists have no recourse to the CQC.
The GPhC is primarily a regulator of pharmacy services, and does not have specific guidance for operating a pharmacy website or for prescribing remotely.
Pharmacists appear to operate in a partial regulatory gap.
Next step for CCGs: co-commissioning pharmacy, dentistry and eye careWhy are pharmacist prescribers not regulated the same as other prescribers?
13 November 2014
There appears to be a gap in the prescribing regulations, writes Dr Tony Steele, medical director of Dr Fox online doctors and pharmacy service. Doctors and all other independent prescriber groups, such as nurse prescribers, work under the auspices of the Care Quality Commission (CQC) - except for pharmacy prescribers.
If a doctor wishes to provide a private diagnostic and prescription service, CQC registration is required. A pharmacist prescriber undertaking similar work is not required to register with the CQC. This may sound like a minor matter, but the CQC has a comprehensive process of registration which looks at all aspects of service provision. Registration usually involves an inspection, interview, a fee and annual reporting, audit and re-inspection.
The General Pharmaceutical Council (GPhC), which oversees pharmacy prescribing, does not have a similar process for registering and monitoring pharmacy prescribing services. Pharmacist prescribers are not revalidated in the same way as doctors.
This anomaly throws up some interesting questions for regulators, particularly in the internet age. Pharmacists are increasingly prescribing online and not always to the same standards. The patients of pharmacists have no recourse to the CQC.
The GPhC is primarily a regulator of pharmacy services, and does not have specific guidance for operating a pharmacy website or for prescribing remotely.
Pharmacists appear to operate in a partial regulatory gap.
DUTY OF CANDOUR
Government publishes fundaments standards
http://nhs.us5.list-manage.com/track/click?u=fe51aa41404cfb64f7d454491&id=82af43a0d9&e=b6863b281b
The Government has published the fundamental standards regulations. They include two regulations – the Duty of Candour and the Fit and Proper Person requirement for directors – which will come into force on 27 November for NHS Trusts, Foundation Trusts and some special health authorities.
The Duty of Candour and the Fit and Proper Person requirement for directors will also be extended to all other providers from April 2015 via additional regulations, pending Parliamentary approval
Government publishes fundaments standards
http://nhs.us5.list-manage.com/track/click?u=fe51aa41404cfb64f7d454491&id=82af43a0d9&e=b6863b281b
The Government has published the fundamental standards regulations. They include two regulations – the Duty of Candour and the Fit and Proper Person requirement for directors – which will come into force on 27 November for NHS Trusts, Foundation Trusts and some special health authorities.
The Duty of Candour and the Fit and Proper Person requirement for directors will also be extended to all other providers from April 2015 via additional regulations, pending Parliamentary approval
|
HWBBs - GETTING THE MESSAGE OUT THERE
12 pages This Guide was written in response to requests from people working with Health and Wellbeing Boards, who want to use social media effectively to help the Boards shape policy, explain decisions and deliver objectives. |
|
GUIDE FOR LOCAL HEALTHWATCH MEMBERS OF HWBBs - LGA
‘Healthwatch: On the board toolkit’ published by LGA 10 November 2014 This toolkit is part of the LGA's 'Healthwatch: On the Board' series, designed as a learning aid to support local Healthwatch representatives on their health and wellbeing board (HWB). See more at: http://www.local.gov.uk/web/guest/health-and-wellbeing-boards/-/journal_content/56/10180/6704111/PUBLICATION#sthash.OmvsKr8q.dpuf |
£10b MUST BE SAVED ...
Health secretary Jeremy Hunt sets out measures to deliver up to £10bn in savings across the NHS by 2020 in a speech responding to NHS England's blueprint for the health service. How Jeremy Hunt hopes to make £10bn savings:
Health secretary Jeremy Hunt sets out measures to deliver up to £10bn in savings across the NHS by 2020 in a speech responding to NHS England's blueprint for the health service. How Jeremy Hunt hopes to make £10bn savings:
- Reduce £2.5bn annual cost of avoidable harm
- Minimise prescribing errors - possible £551m saving
- Cut wastage of unused drugs - possible £150m saving
- Improve procurement - possible £1.5bn saving
- Bring down £2.5bn annual agency staff bills
- Sell off surplus land and estates - unused land in London alone worth £1.5bn
- Recoup £500m a year from visitors and migrants by middle of next parliament
- Reduce administration costs - £300m saving target for 2015/16
- Reduce spend on management consultants – currently around £500m a year
- Make better use of IT
£60.00 PER GP HOME VISIT TO OUT-OF-AREA PATIENTS
GPs will be paid £60 per home visit to patients registered with an out-of-area practice under the new GP choice scheme being rolled out in January, service specifications released today have revealed. [http://www.england.nhs.uk/wp-content/uploads/2014/11/gp-con-guidance-out-area-reg.pdf]
The specifications for the new enhanced service so said that GPs will be paid £16 for conducting a appointments in practice with a patient registered elsewhere, which is more than had been previously expected, in that one area team had arrangements in place to pay £40 for home visits and £11 for emergency appointments.
In separate guidance on the GP choice scheme unveiled by NHS England today it also revealed that in order to pay for the provision of local care to these patients it may have to reduce payments to the GP practices that are registering out of catchment area patients without the responsibility for home visits.
NHS England admitted that it only expected 0.4% of the population to use the new patient choice scheme, which allows them to register out of their area, including registering with practices closer to their work.
The details of this new enhanced service come after NHS England was forced to delay the scheme from 1 October this year to 5 January, following concerns raised by the GPC that practices had not been given enough time to prepare.
GPs will be paid £60 per home visit to patients registered with an out-of-area practice under the new GP choice scheme being rolled out in January, service specifications released today have revealed. [http://www.england.nhs.uk/wp-content/uploads/2014/11/gp-con-guidance-out-area-reg.pdf]
The specifications for the new enhanced service so said that GPs will be paid £16 for conducting a appointments in practice with a patient registered elsewhere, which is more than had been previously expected, in that one area team had arrangements in place to pay £40 for home visits and £11 for emergency appointments.
In separate guidance on the GP choice scheme unveiled by NHS England today it also revealed that in order to pay for the provision of local care to these patients it may have to reduce payments to the GP practices that are registering out of catchment area patients without the responsibility for home visits.
NHS England admitted that it only expected 0.4% of the population to use the new patient choice scheme, which allows them to register out of their area, including registering with practices closer to their work.
The details of this new enhanced service come after NHS England was forced to delay the scheme from 1 October this year to 5 January, following concerns raised by the GPC that practices had not been given enough time to prepare.
COMPLAINTS - SOCIAL CARE, ETC.
11 pages
Nadine Dorries (Mid Bedfordshire, Conservative)
To ask the Secretary of State for Health, what steps his Department takes to ensure that local authorities are aware of their obligations to investigate complaints about poor-quality social care; and what assistance the Government provides to help them meet those obligations.
Norman Lamb (The Minister of State, Department of Health; North Norfolk, Liberal Democrat)
Each local authority is responsible for the quality of social care services it commissions. There is no national register or oversight of complaints in social care.
11 pages
Nadine Dorries (Mid Bedfordshire, Conservative)
To ask the Secretary of State for Health, what steps his Department takes to ensure that local authorities are aware of their obligations to investigate complaints about poor-quality social care; and what assistance the Government provides to help them meet those obligations.
Norman Lamb (The Minister of State, Department of Health; North Norfolk, Liberal Democrat)
Each local authority is responsible for the quality of social care services it commissions. There is no national register or oversight of complaints in social care.
However, local authorities are required, pursuant to the Local Authority Social Services and National Health Service (England) Regulations 2009, to keep a record of each complaint received, the subject matter and outcome and timescales for responding. They are also obliged to make a summary of this information available to the public via an annual report. The Government believes that we should be committed to ensuring the system for resolving complaints about care is compassionate, personal, responsive, timely and ensures lessons are learned.
The Department established a national complaints programme board in December 2013. A comprehensive programme has been developed with national partners, including the Care Quality Commission (CQC), NHS England, Healthwatch England, the Parliamentary and Health Service Ombudsman, the Local Government Ombudsman, the Local Government Association, Monitor and the NHS Trust Development Association, to bring about important changes to the way complainants are supported and complaints are handled across the health and social care systems.
The Department established a national complaints programme board in December 2013. A comprehensive programme has been developed with national partners, including the Care Quality Commission (CQC), NHS England, Healthwatch England, the Parliamentary and Health Service Ombudsman, the Local Government Ombudsman, the Local Government Association, Monitor and the NHS Trust Development Association, to bring about important changes to the way complainants are supported and complaints are handled across the health and social care systems.
HAPIA NEGOTIATES LHW ACCESS TO IMMIGRATION REMOVAL CENTRES
Healthcare of those in Immigration Removal Centres comes under the scrutiny of LHW.
Download the letter from the Head of Detention Operations Immigration Enforcement - dated 10 November 2014 - to Malcolm Alexander, Chair, HAPIA in response to his letter - dated 16 July 2014
Healthcare of those in Immigration Removal Centres comes under the scrutiny of LHW.
Download the letter from the Head of Detention Operations Immigration Enforcement - dated 10 November 2014 - to Malcolm Alexander, Chair, HAPIA in response to his letter - dated 16 July 2014
SCRUTINY - POST FRANCIS
6 pages
- Use information that is available: media reports, public Board papers,
complaints data and published statistics about health and care outcomes.
- Collaborate to avoid duplication and complement the work of others.
- Training and knowledge will lead to improved performance
6 pages
- Introduction
- Responding to Francis
- What is the briefing about?
- What specific recommendations were made for council scrutiny?
- Use information that is available: media reports, public Board papers,
complaints data and published statistics about health and care outcomes.
- Collaborate to avoid duplication and complement the work of others.
- Training and knowledge will lead to improved performance
- Conclusion
SCRUTINY OF EYE HEALTH - WHAT TO BE AWARE OF ...
16 pages
16 pages
- Has an eye health needs assessment been carried out in your local area?
- Starting young – is a children’s vision screening service available?
- What eye health services are currently available?
- What steps have been taken to ensure that excluded groups have access to regular sight testing?
- What work has been carried out to reduce the number of people with cataracts, glaucoma or Age related Macular Degeneration (AMD) in accordance with the Public Health Indicator for preventable sight loss?
- Is a diabetic retinopathy screening programme currently in place?
- Is there a local eye health network in your area?
- Clinical Council for Eye Health Commissioning
APPS FOR ALL?
The NHS is set to make a fresh push to encourage GPs to prescribe the use of 'apps' and other digital tools in a key strategy document next week, according to an NHS England National Director.
Tim Kelsey, the body’s National Director for Patients and Information, said the proposals, including an “NHS app store”, would be laid out in a strategy document called Personalising Health and Care 2020. The idea of accredited apps was included in the NHS Five Year Forward View, published by NHS England last month. The document said there would be “an expanding set of NHS accredited 'health apps' that patients will be able to use to organise and manage their own health and care; and the development of partnerships with the voluntary sector and industry”.
Plans for NHS accredited apps were also outlined in the 2012 Department of Health paper, The power of information: Putting all of us in control of the health and care information we need. The paper said: “To accelerate development and use of innovative information based services – including mobile apps – for the benefit of people, professionals and organisations, a partnership with industry and with health and care providers will now step up active work towards the introduction, publication and adoption, by no later than 2015, of interface standards.”
The NHS is set to make a fresh push to encourage GPs to prescribe the use of 'apps' and other digital tools in a key strategy document next week, according to an NHS England National Director.
Tim Kelsey, the body’s National Director for Patients and Information, said the proposals, including an “NHS app store”, would be laid out in a strategy document called Personalising Health and Care 2020. The idea of accredited apps was included in the NHS Five Year Forward View, published by NHS England last month. The document said there would be “an expanding set of NHS accredited 'health apps' that patients will be able to use to organise and manage their own health and care; and the development of partnerships with the voluntary sector and industry”.
Plans for NHS accredited apps were also outlined in the 2012 Department of Health paper, The power of information: Putting all of us in control of the health and care information we need. The paper said: “To accelerate development and use of innovative information based services – including mobile apps – for the benefit of people, professionals and organisations, a partnership with industry and with health and care providers will now step up active work towards the introduction, publication and adoption, by no later than 2015, of interface standards.”
GP-LED HEALTH CENTRES HIT BY NEW DIRECTIVE
Commissioners are using break clauses in APMS Contracts to impose the new arrangements following an NHS England national directive to separate the 8.00am - 8.00pm walk-in services from the registered patients' service at GP-led Health Centres.
The Health Minister has promised to look into the threat so some Practices, which could be made unviable by proposed funding cuts of up to 43%.
Commissioners are using break clauses in APMS Contracts to impose the new arrangements following an NHS England national directive to separate the 8.00am - 8.00pm walk-in services from the registered patients' service at GP-led Health Centres.
The Health Minister has promised to look into the threat so some Practices, which could be made unviable by proposed funding cuts of up to 43%.
GPs WILL NOT CONTROL PRIMARY CARE COMMISSIONING UNDER NEW CCG REFORMS
Papers published ahead of this week’s NHS England Board Meeting (7 pages) detail proposed tough measures to guard against conflicts of interest. The report, written by national director for commissioning strategy Ian Dodge, said CCG decision-making committees would have a lay and executive majority and have a lay chair, putting control out the hands of GPs.
The measures, due to be consulted on if approved at Thursday's board meeting, would be put on a statutory basis.
The ‘significantly enhanced’ measures against conflicts of interest would also see enhanced training for lay members, public registers of interests and decisions, and observer rights for local authority and Health Watch representatives.
Papers published ahead of this week’s NHS England Board Meeting (7 pages) detail proposed tough measures to guard against conflicts of interest. The report, written by national director for commissioning strategy Ian Dodge, said CCG decision-making committees would have a lay and executive majority and have a lay chair, putting control out the hands of GPs.
The measures, due to be consulted on if approved at Thursday's board meeting, would be put on a statutory basis.
The ‘significantly enhanced’ measures against conflicts of interest would also see enhanced training for lay members, public registers of interests and decisions, and observer rights for local authority and Health Watch representatives.
HAPIA CONFERENCE - Thursday, 30 October 2014 ... PowerPoint Presentations
Click here to go directly to the Conference 2014 page to download the Presentations
Click here to go directly to the Conference 2014 page to download the Presentations
|
Letter from: CARE QUALITY COMMISSION in response to a letter sent by Malcolm Alexander, Chair, HAPIA
In terms of:
|